The study conducted by Cindy X. Cai, MD, and colleagues from Wilmer Eye Institute at Johns Hopkins School of Medicine shed light on the correlation between adverse social determinants of health and the severity of rhegmatogenous retinal detachment (RRD). The retrospective cohort study analyzed 700 patients who underwent primary repair of uncomplicated RRD at a single center and found a compelling link between socioeconomic disadvantage and delayed treatment. According to the findings, each decile increase in the Area Deprivation Index (ADI) was associated with higher odds of presenting with worse visual acuity and fovea-involving RRD. This suggests that individuals with lower socioeconomic status may face barriers that prevent them from seeking timely medical care for retinal detachment.
Patients residing in neighborhoods with higher ADI scores were more likely to present with severe RRD, indicating a delay in seeking medical intervention. The study highlighted that for every $1,000 increase in per capita income, there were lower odds of presenting with worse vision. Furthermore, patients living in areas with a higher percentage of workers who drove to work were also at increased risk of presenting with worse vision and fovea-involving RRD. These findings emphasize the impact of socioeconomic disparities on access to healthcare services and the subsequent implications for disease management.
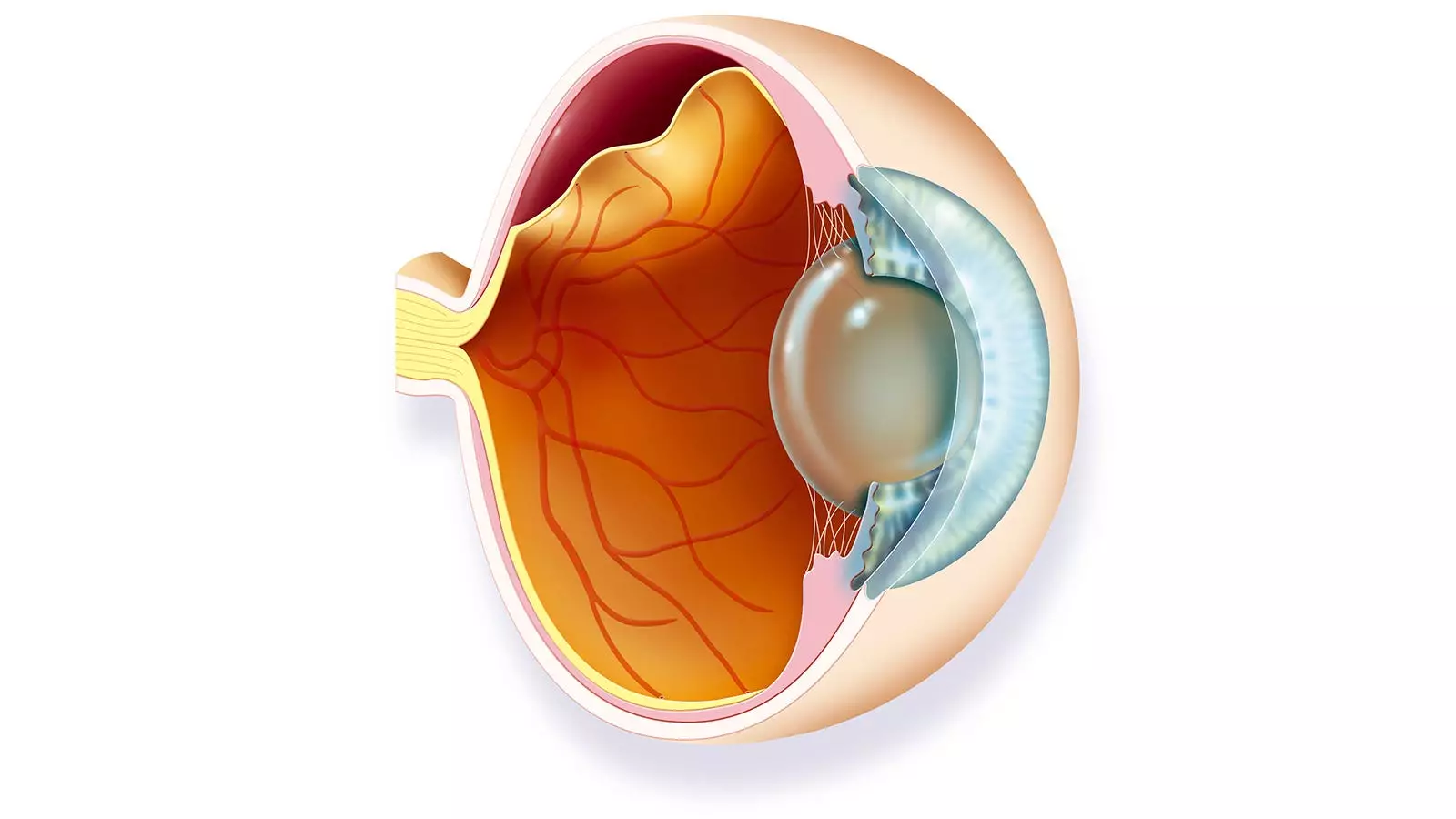
Co-author Sally S. Ong, MD, highlighted the challenges faced by patients with socioeconomic disadvantages in accessing timely care for retinal detachment. Patients lacking access to transportation, time off work, or awareness of the symptoms may delay seeking medical attention until the condition has progressed to a severe stage. Fovea involvement, indicating the advancement of detachment into the central retina, was observed in patients with delayed treatment, resulting in compromised vision. The study underscores the need for interventions to address barriers to care faced by disadvantaged populations and emphasizes the importance of raising public awareness about the signs of retinal detachment.
Healthcare providers are encouraged to educate disadvantaged patients about the significance of prompt treatment for retinal detachment and to collaborate with social workers to facilitate access to care. Strategies such as addressing transportation challenges and raising awareness about the importance of early intervention can help mitigate the impact of social determinants of health on disease outcomes. The study’s implications extend beyond retinal detachment, highlighting the broader issue of healthcare disparities faced by marginalized populations in accessing essential medical services.
The commentary by Patrice M. Hicks, PhD, MPH, and colleagues from the University of Michigan delved into the intersection of patient-level and neighborhood-level factors in exacerbating healthcare disparities. The study’s findings raised questions about the severity of RRD in neighborhoods where more residents relied on driving to work. The speculated lack of public transit options in these areas may hinder individuals without cars from accessing medical care, contributing to delays in treatment and worse outcomes. The researchers emphasized the need to examine nuanced interactions between social determinants of health and healthcare disparities to address systemic barriers to care.
The study underscores the critical impact of social determinants of health on the severity and management of rhegmatogenous retinal detachment. By identifying the link between socioeconomic disadvantage, delayed treatment, and worse visual outcomes, healthcare providers can implement targeted interventions to improve access to care for marginalized populations. Addressing barriers such as transportation challenges, awareness gaps, and socioeconomic disparities is essential in promoting equitable healthcare services and preventing adverse health outcomes related to retinal detachment.
Leave a Reply