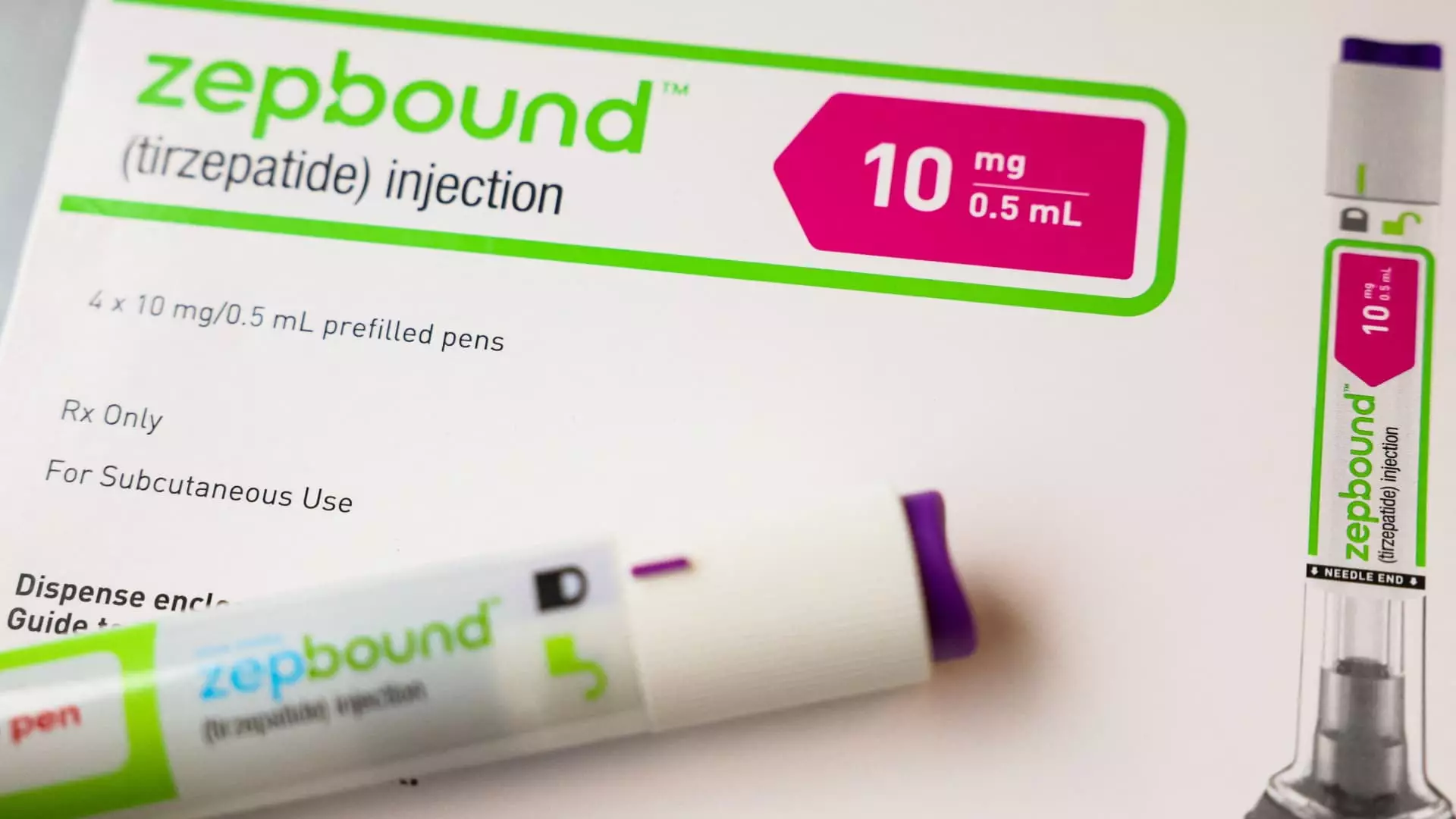
In a significant policy shift, the Centers for Medicare & Medicaid Services (CMS) recently confirmed that Medicare drug plans will include coverage for Eli Lilly’s Zepbound, specifically for patients diagnosed with obstructive sleep apnea (OSA). This decision opens up new avenues for Medicare recipients battling obesity-related health issues and reflects broader trends in the healthcare sector. Zepbound’s approval last month marks a foundational development, particularly given that OSA affects approximately 20 million Americans.
Zepbound’s introduction into the Medicare landscape is particularly noteworthy since it reflects an evolving perspective on how obesity treatments can also mitigate complications from related health conditions. The Affordable Care Act initially limited the scope of coverage for weight loss drugs, requiring these medications to be prescribed not just for obesity, but also for other FDA-approved conditions. The latest development involving Zepbound suggests a gradual re-evaluation of these stringent criteria, acknowledging the multifaceted impact of obesity on patients’ overall health, especially regarding sleep-related issues.
The CMS has explicitly stated that the existing Medicare Part D and Medicaid coverage regulations will apply to Zepbound, indicating a cautious but crucial step forward. However, the coverage is not guaranteed under all circumstances. For Zepbound to be covered, it must be prescribed specifically for obstructive sleep apnea, and there may be additional requirements, such as prior authorization from providers who would need to demonstrate that the medication is being used for its intended purpose. This intricacy reflects a standard approach often seen with high-cost medications where insurance providers seek to balance patient access with the necessity to control costs and ensure appropriate use.
Moreover, Zepbound is uniquely positioned within a competitive market that includes other obesity drugs, such as Novo Nordisk’s Wegovy. The latter is also approved for cardiovascular risk reduction, showcasing a trend where drugs are increasingly being repurposed for multiple conditions. These developments compel an ongoing assessment of how insurance companies and healthcare providers approach medication management and coverage stipulations.
One major concern that arises from this expansion of coverage is the financial burden placed on the healthcare system. Zepbound, which comes with a hefty price tag of around $1,000 per injection without insurance, raises critical questions about the sustainability of such coverage expansion. The Biden administration’s proposed rule to broaden access to weight loss drugs could potentially cost taxpayers upward of $35 billion over the next decade, emphasizing the financial stakes involved in integrating obesity treatments into Medicare and Medicaid offerings. This is an alarming reality that stakeholders must consider as they evaluate the viability of expanding coverage for obesity-related drugs.
On a state level, Medicaid coverage for Zepbound remains multifaceted. State programs can choose whether to cover the drug based on its prescribed condition. For example, if Zepbound is administered for OSA, states must provide coverage if Eli Lilly has entered into the Medicaid drug rebate agreement. However, if prescribed solely for weight loss, states are not legally obligated to include Zepbound in their plans. This variability creates a patchwork coverage system that can confuse patients and providers alike.
As Eli Lilly and its competitors continue investigating their drugs’ applicability to health issues such as fatty liver disease and chronic kidney disease, future FDA approvals could lead to wider coverage under both Medicare and Medicaid. In such a scenario, it’s pivotal to establish clear guidelines and frameworks to ensure that patient access does not compromise the financial integrity of these essential programs.
The approval of Zepbound for OSA represents a significant advancement in the treatment of obesity and its related conditions. While the complexities of drug coverage policies and the associated financial considerations pose significant challenges, this development underscores a larger movement towards integrating obesity management into comprehensive healthcare solutions. As healthcare policy continues to evolve, the focus must remain on balancing effective treatment options with responsible fiscal management, ensuring that every patient has the opportunity to achieve better health outcomes without fear of financial incapacitation.
Leave a Reply