In a recent analysis of the FRAME-AMI trial, fractional flow reserve (FFR) guidance emerged as a potential solution to enhance cost-effectiveness and improve the quality of life for individuals with acute myocardial infarction (MI) undergoing complete revascularization. The findings, published in JAMA Network Open, demonstrated that the implementation of FFR strategy led to an increase in quality-adjusted life-years (QALYs) by 0.06 compared to angiography-guided percutaneous coronary intervention (PCI) of non-culprit lesions. Moreover, FFR guidance resulted in a cumulative total cost savings of $1,208 per patient. These promising results prompted the researchers to consider FFR as a more cost-effective approach for patients with acute MI and multivessel disease.
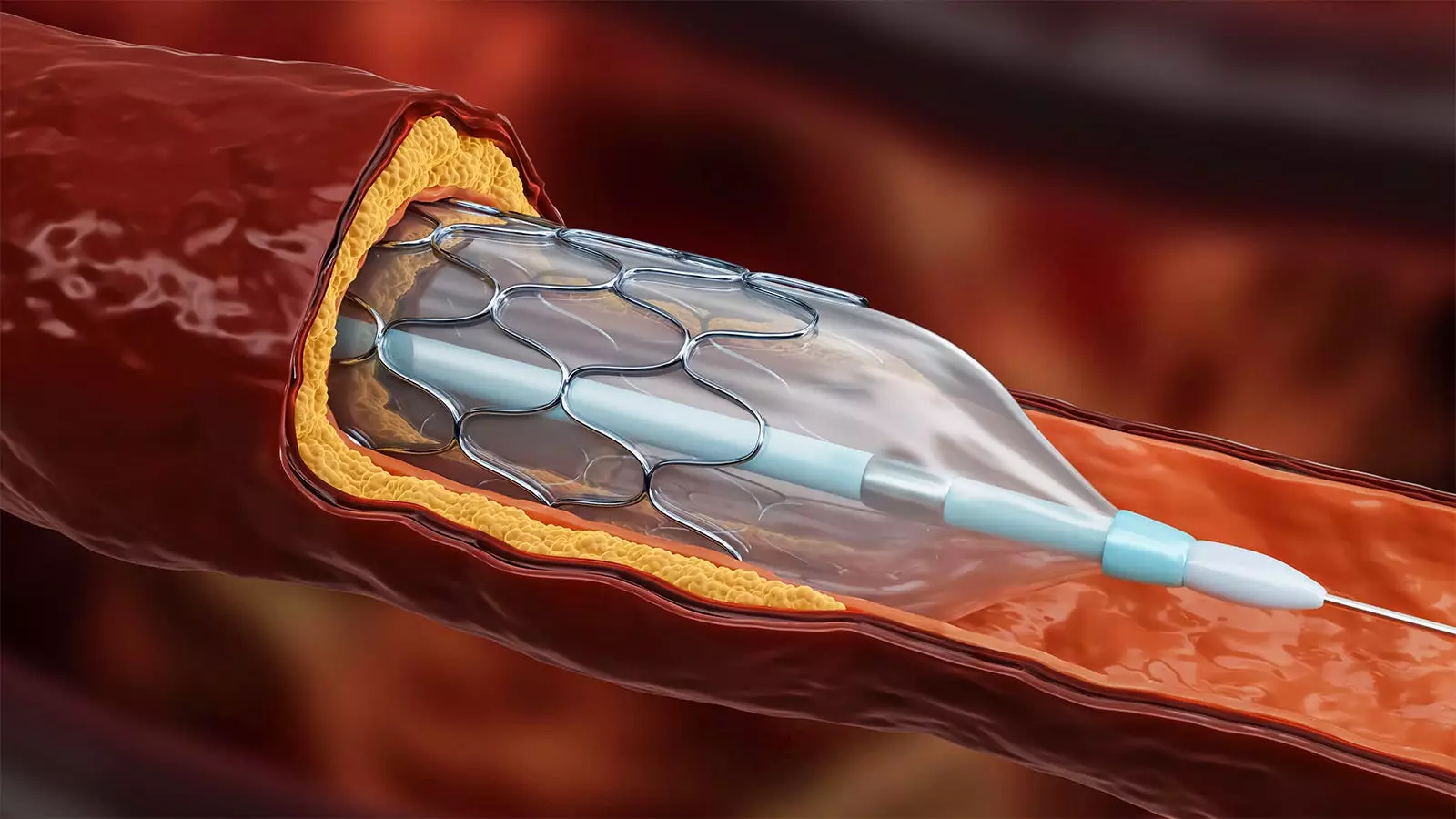
The analysis revealed an incremental cost-effectiveness ratio of -$19,484 and an incremental net monetary benefit of $3,378 for FFR-guided PCI over a four-year time horizon. Importantly, these findings remained consistent across various subgroups and healthcare systems, including those of the United States, Korea, and Europe. The researchers argued that routine angiography-guided PCI for all non-infarct-related artery (IRA) lesions with diameter stenosis greater than 50% may lead to unnecessary procedures with additional stents, increased contrast media usage, and higher risks of procedure-related complications. By contrast, FFR-guided PCI would reduce the need for unnecessary interventions, particularly for functionally insignificant stenosis. The study’s authors emphasized the superiority of FFR-guided PCI for patients with stable ischemic heart disease and those with acute MI and multivessel disease.
While the FLOWER-MI trial did not find FFR to be superior to angiographic guidance, the main results of the FRAME-AMI trial strongly favored the use of FFR guidance in determining nonculprit lesions requiring intervention. The study participants randomized to FFR guidance underwent PCI for non-IRA lesions in 64.1% of cases, compared to 97.1% in the angiography-guided group. Remarkably, deferral of PCI based on FFR provided similar or superior clinical outcomes when compared to angiography-guided PCI. These findings highlight the potential of FFR-guided PCI to reduce rates of non-IRA PCI, resulting in significant cost savings and more efficient utilization of medical resources without compromising patient prognosis.
The cost-effectiveness data provided by the FRAME-AMI trial hold considerable importance in this evolving clinical paradigm. Healthcare practitioners may be inclined to adopt an FFR-based strategy for achieving complete revascularization in patients with acute MI, as it may help combat rising costs while improving clinical outcomes. However, the authors acknowledged the need for larger trials powered for hard outcomes to further assess the preferred strategy in this context. They also noted that FFR-guided complete revascularization in the acute MI population demonstrated cost-effectiveness across diverse healthcare systems worldwide. Consequently, these findings could potentially inform future policies regarding the management of acute MI.
Although the FRAME-AMI trial provides valuable insights, certain limitations warrant consideration. Notably, the trial excluded individuals with left main coronary artery disease or chronic total occlusion in non-IRA lesions. Additionally, the study relied on limited country-level healthcare system data, which may limit the generalizability of the findings. Furthermore, the COVID-19 pandemic necessitated an early termination of the study.
Moving forward, ongoing trials, such as FULL REVASC, OPTION-STEMI, and COMPLETE 2, will contribute to the growing body of evidence in this domain. Continued research will aid in better understanding the role of FFR-guided PCI in achieving complete revascularization and optimizing the management of acute MI patients.
The implementation of FFR guidance in nonculprit lesion intervention for individuals with acute MI has shown promise in increasing cost-effectiveness and improving quality of life. The analysis of the FRAME-AMI trial demonstrated the superiority of FFR-guided PCI over angiography-guided PCI, with favorable outcomes across various healthcare systems. By reducing unnecessary interventions and optimizing resource utilization, FFR-guided PCI offers a potential solution to the challenges posed by rising healthcare costs. Further research and larger trials will provide a deeper understanding of the role of FFR-guided PCI in optimizing patient outcomes and informing evidence-based clinical guidelines.
Leave a Reply