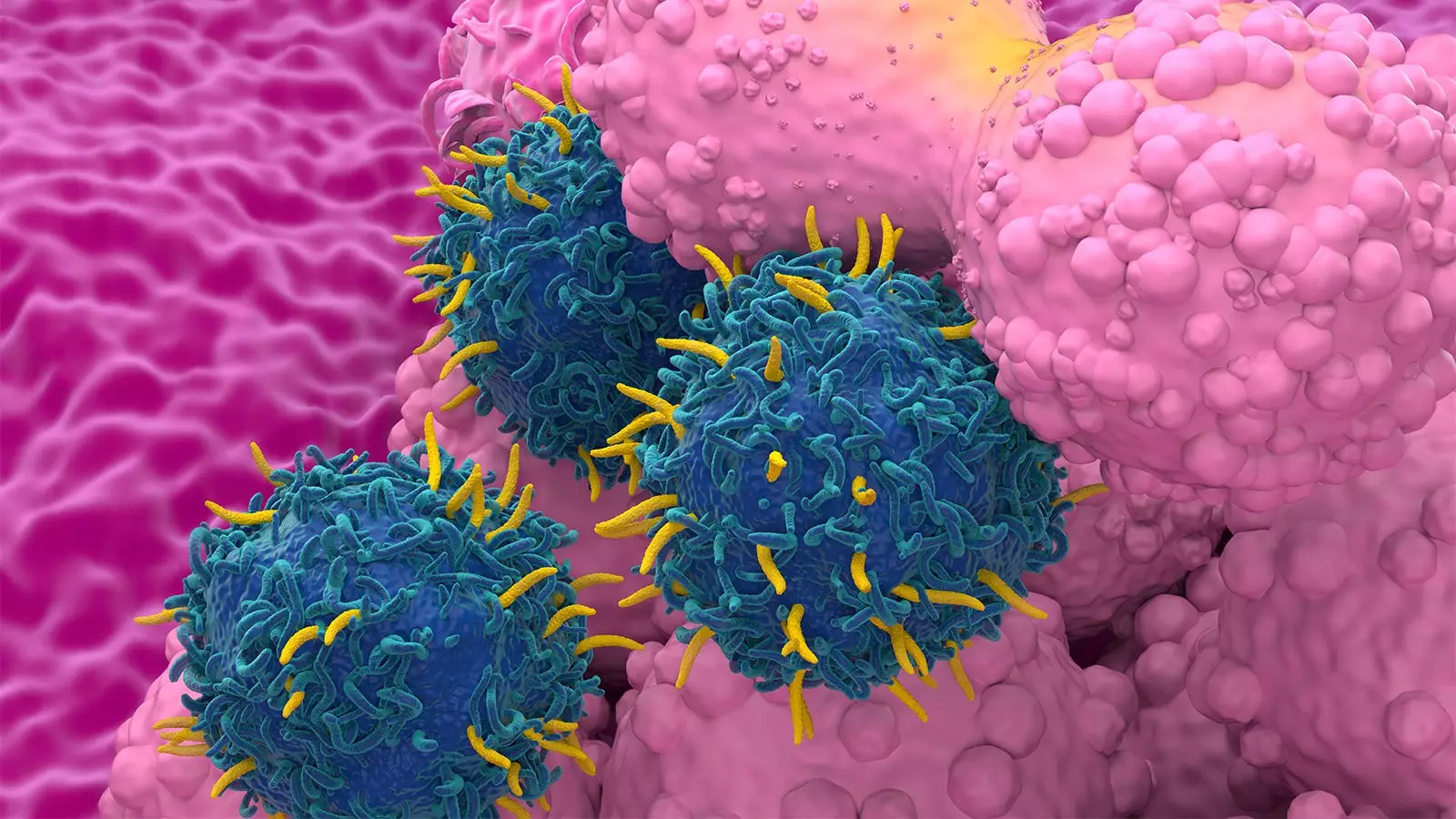
CAR T-cell therapy has emerged as a promising treatment option for patients with certain types of cancer, offering new hope for those who have exhausted standard-of-care options. However, recent concerns have been raised about the risk of developing second primary malignancies (SPMs) following CAR T-cell therapy. A systematic literature review and meta-analysis conducted by researchers shed light on this issue, providing valuable insights into the safety profile of CAR T-cell therapy.
The analysis included data from 5,517 patients with a median follow-up of 21.7 months, revealing a 5.8% rate of SPMs. Interestingly, this rate remained consistent across different types of diseases treated and CAR T-cell products used. Factors such as study setting, duration of follow-up, and the number of prior therapies were found to be associated with a higher risk of SPMs. Moreover, a comparison of CAR T-cell therapy with standard-of-care treatments showed similar rates of SPMs, suggesting that the risk may not be unique to CAR T-cell therapy.
The findings challenge the notion of an increased risk of SPMs with CAR T-cell therapy relative to other treatment modalities. This calls into question the need for a black-box warning label by the FDA, which was prompted by reports of SPMs in CAR T-cell therapy recipients. The authors emphasize the importance of interpreting the data cautiously and considering potential biases in adverse event reporting. They underscore the need for more long-term data to better understand the factors contributing to SPM development in CAR T-cell patients.
To address gaps in understanding, researchers conducted a comprehensive review of published literature and performed a meta-analysis of relevant studies. The analysis included a large cohort of patients across clinical trials and real-world settings, providing a robust assessment of the SPM risk associated with CAR T-cell therapy. Notably, the most common SPMs observed were hematologic malignancies, solid tumors, and non-melanoma skin cancers, with T-cell malignancies accounting for a small proportion of cases.
The study findings have important implications for patient care, as they highlight the need to educate patients about the potential risks associated with CAR T-cell therapy. Providers should be prepared to address patient concerns and help them navigate treatment decisions based on the available data. The authors stress the importance of considering confounding factors such as patient age, treatment history, and follow-up duration when assessing SPM risk in CAR T-cell therapy recipients.
The risk of developing SPMs following CAR T-cell therapy is not significantly higher than that associated with standard-of-care treatments. While important considerations remain regarding data interpretation and patient counseling, the findings provide reassurance about the safety profile of CAR T-cell therapy. Continued research and surveillance will be crucial in further elucidating the long-term effects of this innovative treatment approach.
Leave a Reply