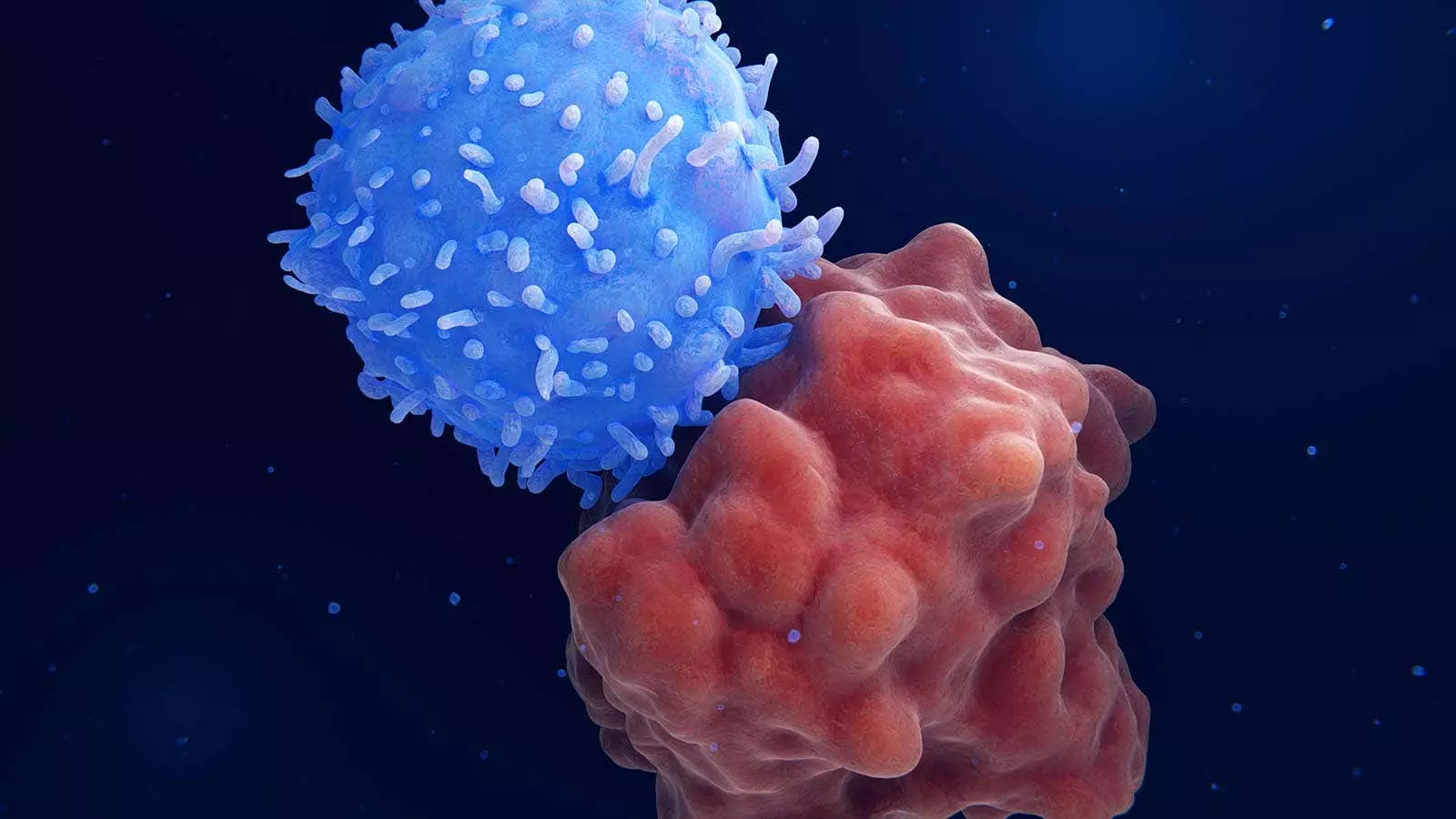
A recent study conducted by Chinese researchers introduced a novel treatment approach for patients with relapsed or refractory hematologic cancers. This strategy combines sequential CD7 chimeric antigen receptor (CAR) T-cell therapy with haploidentical hematopoietic stem-cell transplantation (HSCT), without the use of graft-versus-host disease (GVHD) prophylaxis. The findings of this study, published in the New England Journal of Medicine, shed light on the potential of this innovative procedure in improving outcomes for patients who are ineligible for conventional allogeneic HSCT.
The study, which included 10 patients with relapsed or refractory hematologic cancers, demonstrated promising results following the combination of CAR T-cell therapy and haploidentical HSCT. After receiving CAR T-cell therapy, all patients achieved complete remission, with nine showing minimal residual disease (MRD)-negative incomplete hematologic recovery. Subsequently, nine patients underwent haploidentical HSCT within 1 month, resulting in six patients maintaining MRD-negative complete remission. The estimated 1-year overall survival rate was reported to be 68%, with a disease-free survival rate of 54%.
The rationale behind the use of this all-in-one approach lies in the expression of CD7 in approximately 30% of acute myeloid leukemia (AML) cases. By utilizing CAR T-cell therapy as a bridge to allogeneic HSCT, the researchers aimed to achieve long-term tumor elimination while reducing the risk of relapse. The unique aspect of this strategy is the avoidance of pre-HSCT myeloablation and GVHD prophylaxis agents, which could potentially compromise the antitumor effects of CAR T cells. Additionally, this approach targeted patients who were unfit for allogeneic HSCT, offering them a new treatment option with potentially favorable outcomes.
The 10 patients included in the study were enrolled in either a clinical study of donor-derived CD7 CAR T cells or a compassionate-use program providing access to universal CD7 CAR T cells. These patients had relapsed or refractory CD7-positive leukemia or lymphoma and met specific eligibility criteria for the all-in-one strategy. The majority of patients had AML, with a median age of 56.5 years and a history of extensive prior therapy. The study observed a median time from CAR T-cell infusion to HSPC infusion of 19 days, with most patients experiencing manageable cytokine release syndrome (CRS) and a low incidence of GVHD.
Despite the promising outcomes observed in this study, challenges such as infections and treatment-related complications were encountered in some patients. The researchers acknowledged the need for further research and larger studies to validate the efficacy and safety of this innovative treatment approach. Additionally, future investigations may explore the use of dual CAR T-cell constructs targeting multiple antigens, as well as the potential application of this strategy in newly diagnosed AML cases.
The combination of sequential CD7 CAR T-cell therapy and haploidentical HSCT represents a groundbreaking strategy for patients with relapsed or refractory hematologic cancers. While preliminary, the results of this study offer hope for advancing treatment paradigms in challenging malignancies with poor prognoses. Continued research in this field may pave the way for improved outcomes and novel therapeutic approaches in the management of hematologic cancers.
Leave a Reply