In the ongoing saga of NHS strikes and political maneuvering, it’s clear that surface-level reforms often mask a deeper failure to address the fundamental issues plaguing the healthcare system. Governments, including the current Labour administration, have repeatedly positioned themselves as champions of progress, touting long-term plans and ambitious reforms as evidence of commitment. However, these plans are often built on shaky foundations—reliant on the goodwill of exhausted and underpaid staff, and susceptible to the destabilization that comes with unaddressed grievances. The recent negotiations between the health secretary and the BMA reveal a recurring pattern: promises of stability are mere illusions when the core issues of fair compensation and staff morale remain unresolved.
The political spectacle often revolves around blame-shifting rather than genuine problem-solving. The government claims to have made concessions—pointing to a claimed 29% pay rise—yet the medical workforce vehemently disputes this, emphasizing years of underpayment and inflation of expectations. Meanwhile, the narrative becomes increasingly polarized, with each side accusing the other of risking patients’ lives to serve political ends. The truth, however, is that both narratives are incomplete; neither fully addresses the systemic failures that render these disputes inevitable, nor does either side truly prioritize the needs of patients over political theater.
The Myth of Localized Decision-Making as a Solution
In an attempt to diffuse blame and soften the blow of industrial action, policymakers have advanced their latest strategy: decentralizing decision-making. Allowing local trust leaders to determine which services remain available is presented as a pragmatic solution—an acknowledgment that frontline managers understand their staff and patients better than distant, central authorities. This approach, in theory, promises to mitigate chaos and prioritize urgent care without halting all non-critical activities.
However, beneath this façade lies a dangerous assumption—that local leaders will exercise good judgment consistently and that they can adequately triage without compromising safety. History has shown that when resources are stretched thin, and staff morale is already battered, such decentralization tends to become a convenient excuse for partial neglect. Patients with conditions that are not immediately life-threatening often find themselves caught in the crossfire—either waiting longer or facing cancellations that could impact long-term outcomes. It risks creating a two-tier system within the NHS, where some patients’ needs are prioritized at the expense of others’ safety, a premise that is fundamentally flawed.
The Reality of Underfunding and Workforce Exhaustion
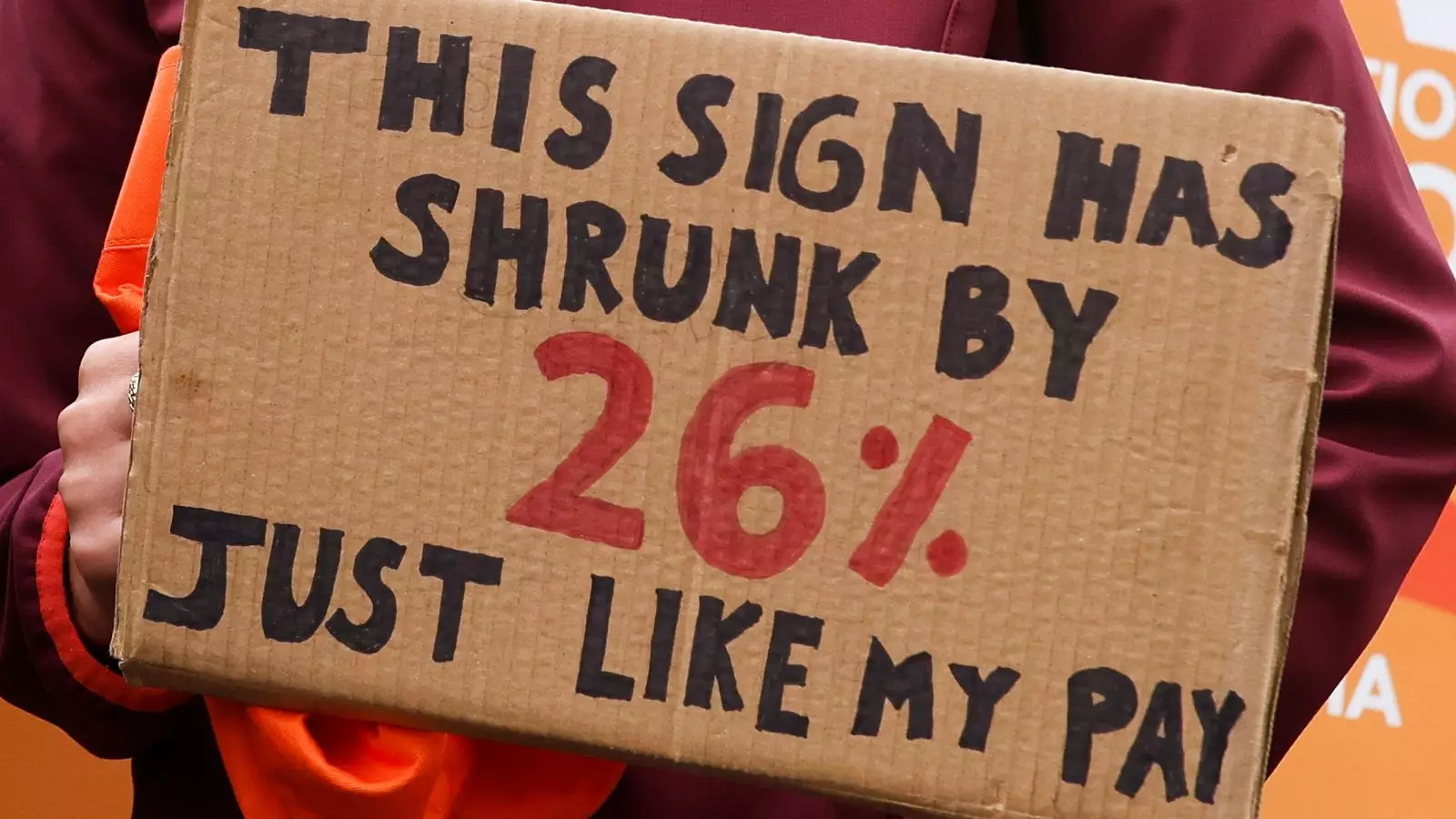
The core dilemma remains: the NHS’s financial and staffing crisis is not a recent phenomenon; it’s a culmination of years of neglect, underfunding, and unrealistic political promises. The BMA’s call for a 26% pay restoration reflects a sense of betrayal—being underpaid for nearly two decades while inflation and operational costs have soared. Their demand isn’t merely about fairness; it’s about survival, acknowledging that the current remuneration does not reasonably compensate the doctors’ expertise, dedication, or the immense pressure they face daily.
Conversely, the government’s stubborn insistence that salaries have already been raised risks overlooking the qualitative gap between pay levels and staff wellbeing. When healthcare professionals feel undervalued, morale plummets, and the resulting burnout exacerbates the staffing crisis. The narrative of “restoring NHS glory” becomes hollow when the people tasked with delivering care feel disposable. It’s a cycle of broken promises—investments announced to placate the public, only to fall short of addressing the systemic issues that fuel strikes and frustration.
The Power of Political Rabble-Rousing
The current political atmosphere amplifies the conflict, turning it into a contest of narratives rather than solutions. The government’s attempt to portray the strikes as reckless or opportunistic neglects the reality that these actions are symptoms of a deeper malaise. Public support wanes, polarized by accusations of endangering patients and political grandstanding. As leaders dig in their heels, the likelihood of genuine compromise diminishes.
This environment fosters a dangerous cycle: each side perceives the other as primarily responsible for chaos, leading to increasingly aggressive rhetoric. Pitting public opinion against healthcare workers, or vice versa, only inflames tensions further. The truth is that without addressing the core issues—funding, staffing, and long-term planning—this cycle of strikes and political blame will persist indefinitely. The NHS’s future hinges on bold, honest leadership willing to confront uncomfortable truths and reject superficial solutions that only serve short-term political gains.
Leave a Reply