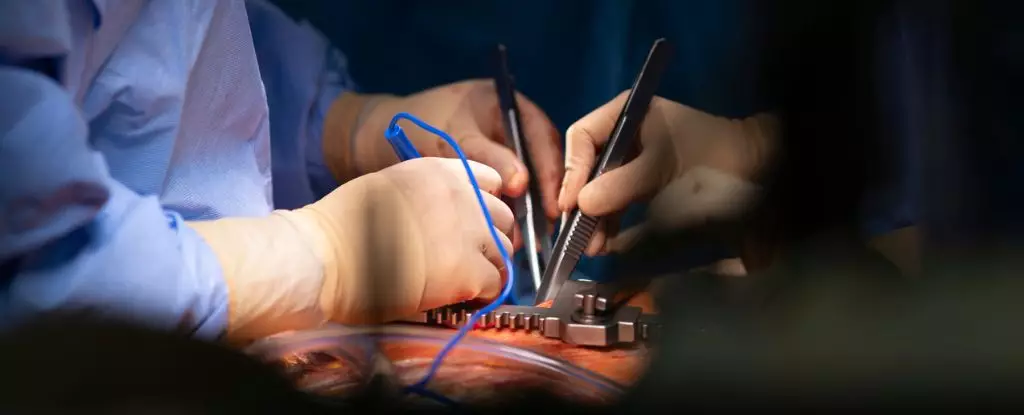
Modern medicine continues to push the boundaries of what is conceivable, especially in the realm of organ transplantation. The groundbreaking work at Duke University, where surgeons successfully resuscitated a heart that had ceased beating for over five minutes, exemplifies this relentless pursuit of innovation. This achievement, which allowed for the transplantation of a seemingly “dead” organ into a fragile infant, underscores a remarkable convergence of technology and hope.
Yet, even as these advances promise salvation for hundreds of children languishing on transplant waiting lists, they also entwine us in complex ethical dilemmas. Is it truly justifiable to manipulate the dying state of a donor’s organ to maximize usable resources? Does this practice blur the line between life and death, casting shadows over the moral foundations of medical ethics? Such questions shouldn’t be dismissed as mere philosophical musings; they strike at the core of our societal values regarding dignity, autonomy, and the definition of death itself.
Redefining Death: When Does Life End?
The crux of the debate hinges on how we define death—a concept that now appears disturbingly fluid in the wake of these technological strides. Critics argue that re-animating a heart post-circulatory death raises serious questions about the legitimacy of declaring death and adhering to traditional standards. When a heart is restarted in a donor after hours of absent circulation, some contend that the process effectively reverses death, challenging the moral integrity of the donation process.
Supporters, however, argue that such methods can safely expand the donor pool, especially for vulnerable pediatric patients with insurmountable needs. Still, this technical contention masks a deeper moral conflict. Are we inadvertently commodifying life, treating organs not as sacred vessels of human dignity but as commodities to be salvaged and repurposed with minimal regard for the donor’s remaining dignity? These practices demand rigorous ethical scrutiny to prevent the erosion of fundamental human rights and societal trust.
Technological Innovation Versus Ethical Conservatism
A particularly nuanced aspect of current developments is the dichotomy between approaches—those aiming to reanimate the heart immediately on the table and those focusing solely on preservation without revival. Duke’s method, utilizing sophisticated machinery to restart the heart after circulation has stopped, highlights their commitment to saving lives at the expense of traditional death definitions. This method could considerably swell the donor pool, but at what moral cost?
Conversely, Vanderbilt’s technique, which emphasizes preservative measures without reanimation, offers a more ethically conservative approach. By avoiding the revival of the heart until transplantation, they sidestep many of the contentious issues surrounding death declaration. This approach advocates for progress through prudence, emphasizing respect for the donor’s dignity and the boundaries established by our moral frameworks.
The real question is whether technological strides should be pursued at the expense of ethical consistency. Does the potential to save more lives justify expanding the moral gray areas we are already treading? Or does such innovation threaten to undermine the societal consensus on what constitutes a respectful and legitimate end of life?
Balancing Hope and Ethics in Transplant Medicine
The relentless pursuit of medical breakthroughs is fundamentally driven by a desire to alleviate human suffering. But in the quest for victory over death, there is a risk of losing sight of the ethical principles that uphold societal trust. The optimism surrounding on-table reanimation and advanced preservation techniques must be tempered by a critical assessment of their moral implications.
Policymakers, medical professionals, and society at large bear the responsibility to ensure that these innovations do not devolve into reckless experimentation. A balanced approach—embracing scientific progress while firmly anchoring itself in ethical integrity—is essential. We must ask ourselves whether the invaluable gains in saving children’s lives outweigh the potential erosion of moral standards that define the dignity of life and death.
Ultimately, as these technologies become more widespread, the societal consensus on death and organ donation could shift dramatically. Such shifts should not be driven solely by technological capability but must be anchored in robust ethical debate that respects human dignity, individual rights, and the moral fabric of our society.
Leave a Reply