For decades, neuroscientists have regarded glycogen solely as a supporting actor—an energy reserve stored predominantly in the liver and muscles, with minimal consideration of its presence in the brain. This narrow perspective ignored the potential functions that glycogen might serve within neural tissue. Recent groundbreaking research from the Buck Institute, however, turns this assumption on its head, suggesting that stored glycogen in the brain isn’t just a passive backup but might actively partake in neurodegenerative processes. This revelation forces us to re-evaluate longstanding models of brain energy metabolism and their implications for aging and disease progression.
In the context of Alzheimer’s disease—a complex tauopathy characterized by harmful protein accumulations—the role of glycogen has been historically overlooked. The new findings suggest that glycogen isn’t merely an innocent bystander but could be an active contributor to neuronal deterioration. If this holds, it reshapes our understanding of neurodegenerative diseases, emphasizing that metabolic dysregulation within neurons could be part of the causal chain, rather than a mere consequence of aging or pathology.
Deciphering the Dangerous Dance of Tau and Glycogen
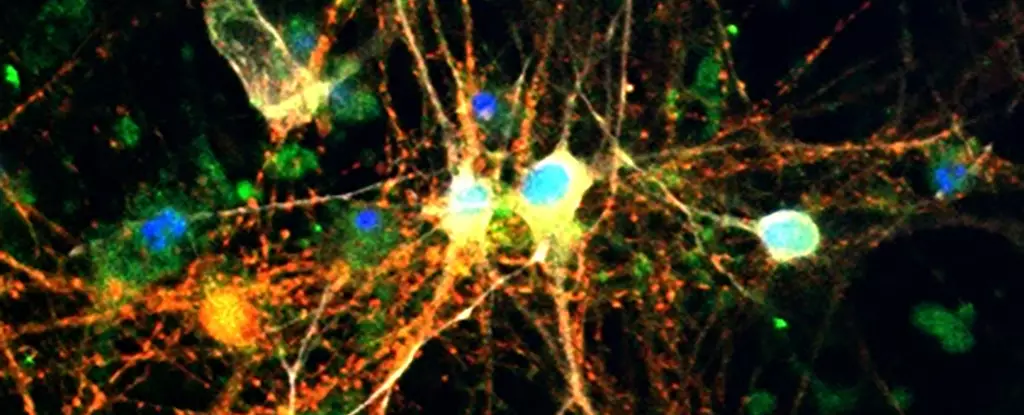
The study uncovers a disturbing relationship between tau proteins and glycogen accumulation. Elevated glycogen levels in tauopathy models—notably in fruit flies and human brain cells—indicate that an aberrant build-up of this sugar reserve correlates with the disease state. More troubling still is the mechanism by which tau proteins impair the normal breakdown of glycogen, creating a vicious cycle that amplifies neuronal stress.
Tau’s interference with glycogen metabolism isn’t harmless; it promotes further aggregation of tau, fuels oxidative stress, and ultimately weakens neurons’ defense systems. The research highlights glycogen phosphorylase (GlyP), an enzyme responsible for converting glycogen into readily usable energy. Increasing GlyP activity in fruit fly models improved glycogen utilization, which resulted in reduced neural damage and even extended lifespan. These results strongly imply that restoring proper glycogen breakdown could be a powerful therapeutic approach—one that fundamentally targets the metabolic underpinnings of neurodegeneration.
Dietary and Pharmacological Strategies Offer Hope—and Caution
The implications of these findings extend beyond molecular biology into the realm of diet and pharmacology. The scientists demonstrated that dietary restriction, especially with reduced protein intake, enhanced GlyP activity in tau-affected flies, prolonging their lives and alleviating brain damage. This aligns with broader evidence supporting caloric restriction and fasting regimens as neuroprotective strategies.
Encouragingly, the team has developed a molecule based on 8-Br-cAMP that mimics the metabolic benefits of dietary restriction, helping to clear glycogen stores and reduce neural damage. This suggests that pharmacological interventions could replicate the effects of diet without the need for drastic lifestyle changes, providing a more accessible avenue for treatment.
The research also hints at exciting connections with existing diabetes medications like GLP-1 receptor agonists, such as Ozempic, which are already targeting metabolic pathways connected to glycogen regulation. These drugs might hold potential in preventing or slowing down neurodegeneration, creating a compelling case for reevaluating their broader therapeutic possibilities.
A Paradigm Shift or a Premature Leap?
While the findings are undeniably compelling, a healthy dose of skepticism remains essential. The leap from fruit fly models and cellular studies to human patients is vast, and many promising discoveries in the lab falter at later stages. There is also the question of whether glycogen accumulation is a cause or consequence of tau pathology—this chicken-and-egg problem complicates the development of targeted therapies.
Moreover, focusing heavily on metabolic interventions risks oversimplifying the multifaceted nature of neurodegenerative diseases like Alzheimer’s, which involve genetic, environmental, and lifestyle factors. While targeting glycogen metabolism is promising, it should coexist with other approaches, not replace them. The danger lies in embracing a one-size-fits-all solution prematurely, outpacing the nuanced complexity of human neurobiology.
Ultimately, this research invites us to reconsider the centrality of cellular metabolism in brain health—not just as a background process but as a critical player in disease progression. If harnessed correctly, it could mark a shift toward more holistic treatment strategies that combine metabolic regulation with molecular and behavioral interventions, propelling us closer to meaningful prevention and cures.
Leave a Reply