In recent years, mouth cancer has become an alarming public health issue in the United Kingdom, reaching a troubling peak of over 10,000 diagnoses. The Oral Health Foundation highlights a staggering 133% increase in cases over the last two decades, an alarming statistic that considerably raises the stakes for public health initiatives. With the number of deaths resulting from mouth cancer also climbing—3,637 in the last year alone—it has never been more critical for individuals and families to understand the risks, symptoms, and essential steps toward prevention.
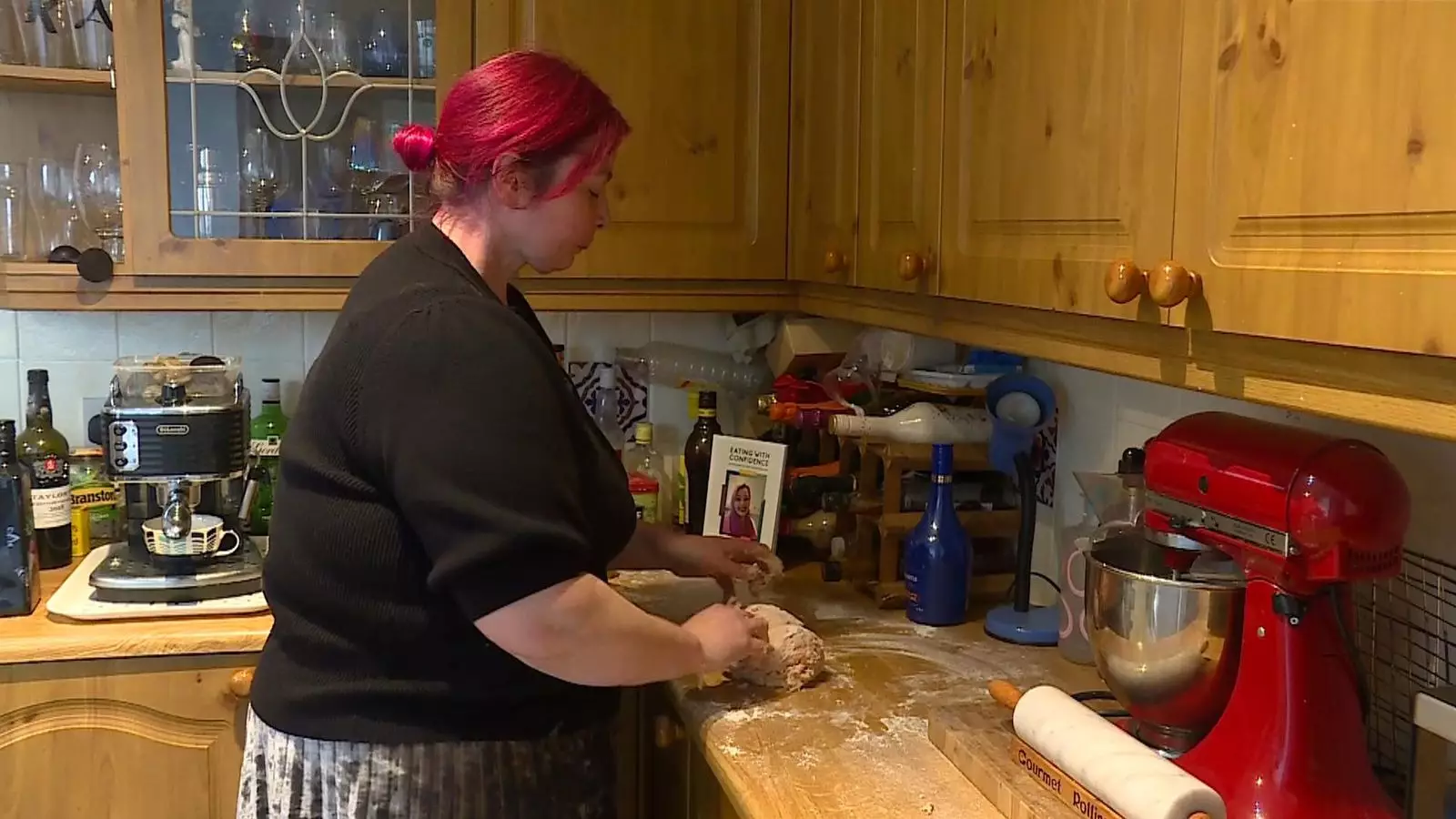
Among those affected by this disease is Laura Marston, a native foodie who once found joy in cooking and baking. Her life came crashing down upon her diagnosis of mouth cancer in 2019. The grim reality of having to navigate life without her tongue has transformed not only her lifestyle but her entire perception of food. “I was told I wouldn’t speak again, I would never eat again,” says Marston, expressing the anguish felt upon hearing doctors deliver life-altering news. It would take months before her condition was accurately diagnosed, tragically leading to her tongue’s removal.
Laura’s plight encapsulates the wider challenges faced by mouth cancer patients. Learning to adapt to a new way of eating and communication, she has become a beacon of hope for others enduring similar struggles. Through these challenges, she authored a cookbook aimed at empowering those with similar conditions to cultivate their love for food despite considerable obstacles.
Mouth cancer can manifest in various forms, with the tongue being a common site for diagnosis—accounting for 31% of cases according to the Oral Health Foundation. Besides the tongue, tonsils and other oral regions such as the lips, gums, and the inside of the cheeks are also frequently affected. The rise in mouth cancer diagnoses calls for immediate action and an urgent awareness campaign among the public.
Dr. Nigel Carter, chief executive of the Oral Health Foundation, urges individuals to be proactive: “Checking for unusual red or white patches, lumps in the neck, and awareness of associated risk factors is paramount.” Risk factors range from traditional lifestyle choices such as smoking and excessive alcohol consumption to the more recently acknowledged connection with the human papillomavirus (HPV).
The demographic most adversely affected by mouth cancer in England appears to be men over the age of 50. The statistics reveal an overwhelming 90% of diagnoses fall within this age bracket, prompting public health officials to target this group through dedicated awareness initiatives.
Indeed, statistics can offer a daunting perspective: as mouth cancer rates rise, a crucial conversation must emerge about prevention, screening, and early detection. Dr. Carter highlights the necessity of diagnosing mouth cancer in its early stages, as many individuals succumb to the disease after receiving late diagnoses.
Government Initiatives and the Need for Change
Meanwhile, governmental bodies are being called upon to act more decisively. The Department of Health and Social Care acknowledges the challenges within the National Health Service, citing higher than average cancer mortality rates as a pressing issue. The government has made commitments to revamp NHS dentistry and expedite cancer diagnoses, but the real impact of these promises will only be evident in time.
As we dissect the rise in mouth cancer cases through compelling personal stories and sobering statistics, it is clear: public awareness is key. Education, communication, and proactive health checks can significantly alter the trajectory of this disease. Laura Marston’s story is a testament to resilience and the imperative need for solidarity and support toward those battling mouth cancer. Only through collective effort can we hope to reverse this growing trend and ensure a healthier future for all.
Leave a Reply