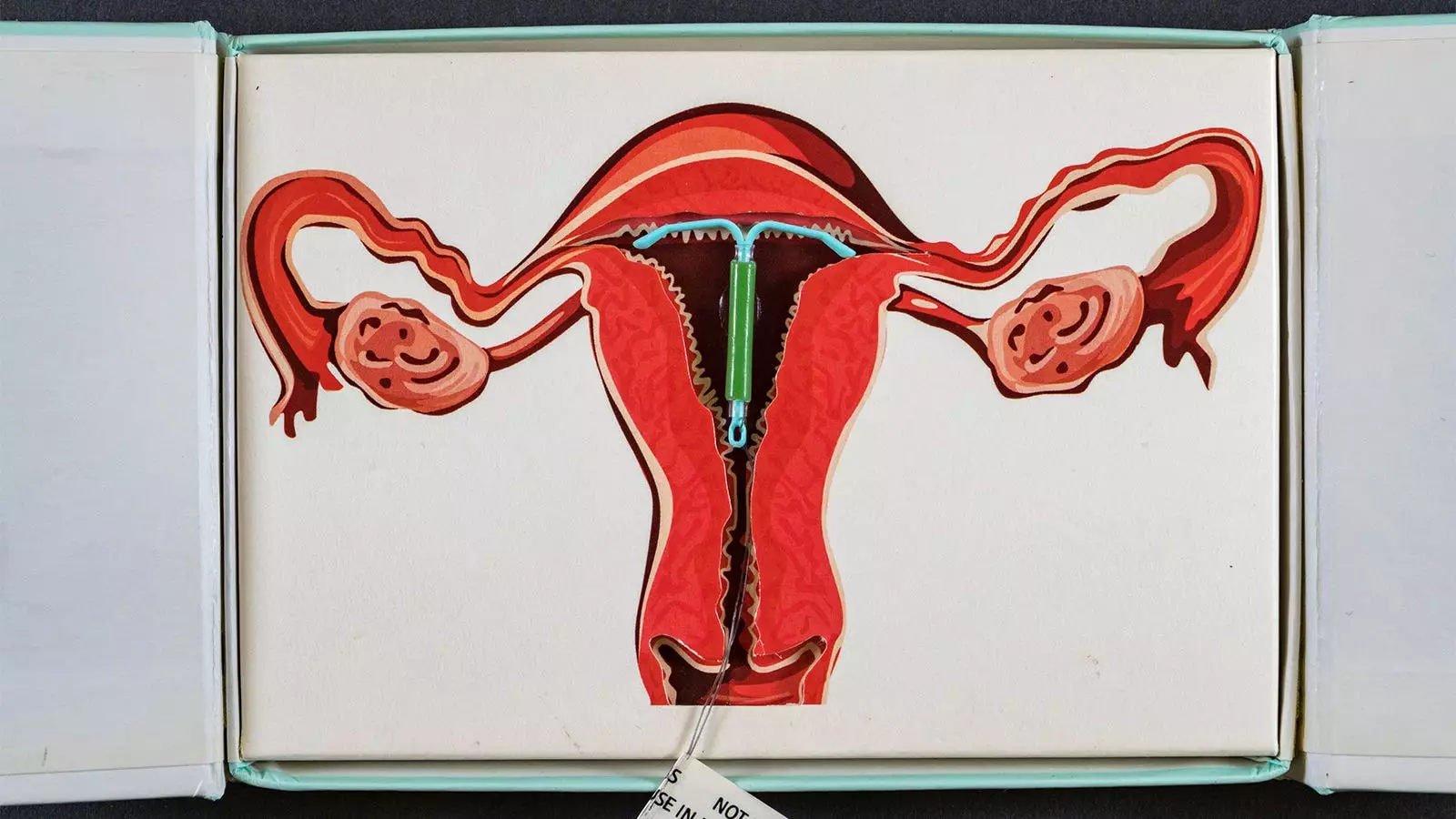
Breast cancer constitutes a significant health challenge, particularly for women who encounter various risk factors, including hormonal contraceptives. A recent Danish registry study has ignited discussions regarding the potential association between levonorgestrel-releasing intrauterine devices (IUDs) and breast cancer risk among women under 50. This novel research reveals that women utilizing these hormonal contraceptives may face a 40% increased risk of developing breast cancer compared to their counterparts who do not use hormonal contraceptives. As the use of long-term contraceptive methods grows, this information prompts a critical reevaluation of public health messaging surrounding IUDs and breast cancer risk.
The comprehensive analysis conducted by Dr. Lina Steinrud Mørch and colleagues at the Danish Cancer Institute involved nearly 78,600 first-time users of levonorgestrel-releasing IUDs from 2000 to 2019. These IUD users were carefully differentiated from a control group of non-hormonal contraceptive users by matching them on key demographic and reproductive health variables. The study tracked outcomes over a mean follow-up period of 6.8 years, revealing a troubling pattern of breast cancer diagnoses associated with prolonged use of the IUD.
The stark findings included 1,617 new breast cancer cases, with a substantial proportion occurring among IUD users. The hazard ratios calculated indicate that the duration of IUD use correlates positively with rising cancer risk: 1.3 for 0-5 years, 1.4 for 5-10 years, and an alarming 1.8 for users who had employed the IUD for over a decade. Such findings have raised legitimate concerns about the long-term implications of hormonal contraceptives on women’s health.
Despite the evident statistical correlations, the study results come with caveats. For instance, the trend indicating an increase in breast cancer diagnoses among users of levonorgestrel-releasing IUDs, while notable, did not achieve statistical significance (P-value of 0.15). This absence of significance suggests that while there appears to be a relationship between IUD use and breast cancer risk, more robust studies are needed to substantiate these findings fully. Moreover, the authors acknowledged potential limitations that might skew the magnitude of the risk, including participant recall bias and the inability to control for unmeasured confounders, such as lifestyle factors or family history.
The implications of these findings emphasize the necessity of comprehensive counseling for women considering hormonal contraceptive options. As the authors articulated, awareness regarding the possible association between the use of IUDs and breast cancer risk should be integrated into discussions about the benefits and risks of long-term contraceptive use. Such transparency is essential in empowering women to make informed decisions about their reproductive health while navigating the complexities of potential health risks.
Furthermore, the increasing use of hormonal contraceptives among young women necessitates a reevaluation of healthcare practices and the dissemination of information. Health professionals must remain vigilant and proactive in providing patients with accurate data, allowing them to weigh the pros and cons effectively. This is particularly crucial as more women are diagnosed with breast cancer at younger ages.
While this Danish study adds essential data to the discussion surrounding hormonal contraceptives and breast cancer, it also highlights the need for further research. Future studies should aim to encompass larger, more diverse populations and consider a broader range of variables that could influence breast cancer risk. Additionally, longitudinal studies are needed to understand the potential long-term health outcomes of various contraceptive methods fully.
As contraceptive technologies and practices evolve, and utilization increases, integrating emerging research findings into clinical guidance is vital. The intersection of hormonal contraceptives and breast cancer risk remains a critical area for ongoing investigation and public health discourse.
Leave a Reply