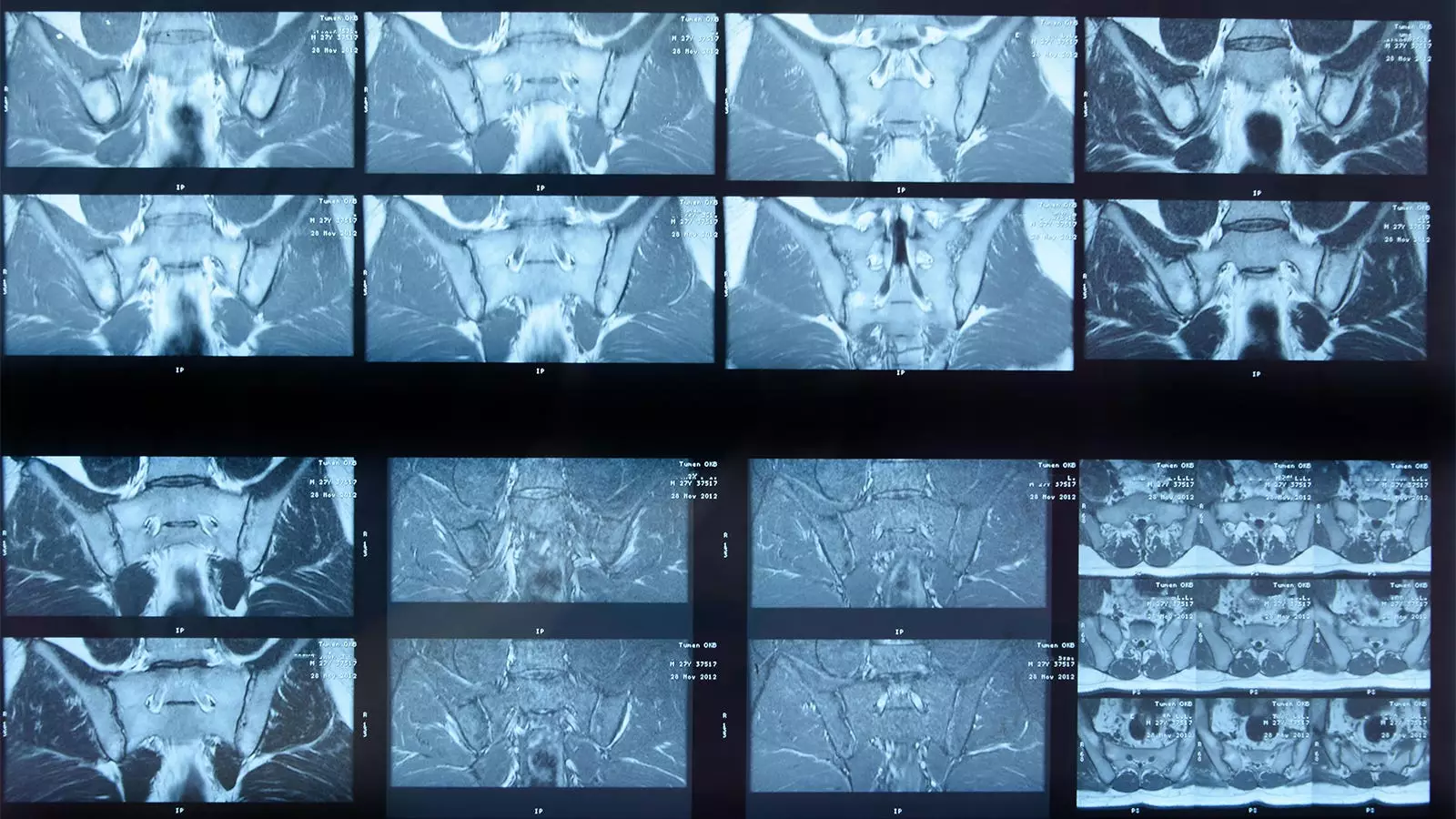
The integration of artificial intelligence (AI) into the realm of medical imaging has ushered in a new era of diagnostic capabilities. One notable instance of this advancement is the emergence of a deep learning algorithm aimed at analyzing MRI scans for the detection of sacroiliac joint (SIJ) inflammation, particularly in patients with axial spondyloarthritis (axSpA). Conducted by a team of researchers led by Joeri Nicolaes, PhD, this study measured the algorithm’s performance against that of human experts, yielding some promising yet mixed results.
The core objective of the research was to validate the efficacy of the AI algorithm using a substantial dataset, involving 731 MRI scans sourced from two clinical trials funded by UCB. These participants, predominantly middle-aged men with a history of axSpA, underwent MRI scans per the trials’ protocols. Each scan was interpreted first by two expert radiologists, with a third called in to resolve disagreements. This structured methodology aimed to mimic real-world clinical environments, where diagnoses can vary significantly between practitioners.
The results presented by Nicolaes and colleagues indicate that the AI algorithm exhibited a degree of concordance with human readers that was “acceptable” but far from perfect. It managed to correctly identify inflammation in 304 cases and agreed with the absence of inflammation in 239 instances. In contrast, the algorithm missed 132 cases of inflammation that the experts identified, while it produced false positives in 56 cases where no inflammation was determined. This led to a calculated absolute agreement of 74%, sensitivity at 70%, and specificity at 81%.
These values suggest an algorithm with moderate reliability, especially when viewed in the context of the challenges faced in interpreting complex MRI images. Nevertheless, the sensitivity and specificity levels indicate room for improvement and emphasize the nascent stage of the technology in clinical environments.
One of the critical factors highlighted by the researchers is the inherent complexity of defining inflammation. The AI’s conservative criteria for identifying SIJ inflammation may not fully align with clinical presentations that human experts consider. For instance, expert readers often rely on additional clinical data, such as C-reactive protein levels or HLA-B27 status, to contextualize their findings. This raises questions about the AI’s ability to incorporate such multifaceted clinical insights into its analysis, a limitation that may hinder its utility in real-world scenarios.
Moreover, the study faced notable limitations regarding the technical specifications of the images processed. The algorithm was unable to analyze scans from 129 participants due to image size issues, suggesting that algorithmic applications must be better adapted to handle diverse imaging conditions seen in routine clinical practice.
While the initial findings of the study present a positive outlook for the applicability of AI in detecting SIJ inflammation, they also underscore the need for ongoing refinement. The algorithm’s creators indicated that the classification criteria for SIJ inflammation have evolved since the algorithm was developed, necessitating revisions to maintain its relevance in contemporary clinical practice. Furthermore, the current iteration lacks the capability to assess structural damage, a critical element in treatment decisions for patients with axSpA.
As the exciting field of medical imaging continues to evolve, it is essential that developers pay attention to real-world clinical requirements. The combination of AI and human expertise must improve to provide not only accurate results but also the interpretative context that skilled clinicians offer.
The exploration of AI’s capabilities in diagnosing SIJ inflammation through MRI scans represents both a significant advancement and a challenge within the field of rheumatology. The findings of this study suggest that while AI has the potential to streamline diagnostic processes and reduce variability in interpretations, it is not yet a replacement for experienced human oversight. As promising as AI algorithms can be, their deployment in clinical settings must be approached with caution and a commitment to continuous improvement, ensuring that patients benefit from the best of both technological and human insights. For the future, the integration of AI systems in diagnostics may require robust feedback mechanisms from clinical environments to refine and augment their decision-making abilities, ultimately enhancing the quality of patient care.
Leave a Reply