Chronic inflammatory demyelinating polyneuropathy (CIDP) is a challenging condition to diagnose and treat effectively. The standard treatments available, such as intravenous immunoglobulin (IVIG), steroids, and plasma exchange, are not always successful for all CIDP phenotypes. As a result, there is a critical need for valid biomarkers that can aid in both diagnosis and treatment of CIDP. According to Dr. Jeffrey Allen of the University of Minnesota, biomarkers are desperately needed to improve the accuracy of diagnosis and understanding of disease activity. The complexity and diversity of CIDP make it difficult to identify biomarkers that can accurately reflect the status of the disease.
The Search for CIDP Biomarkers
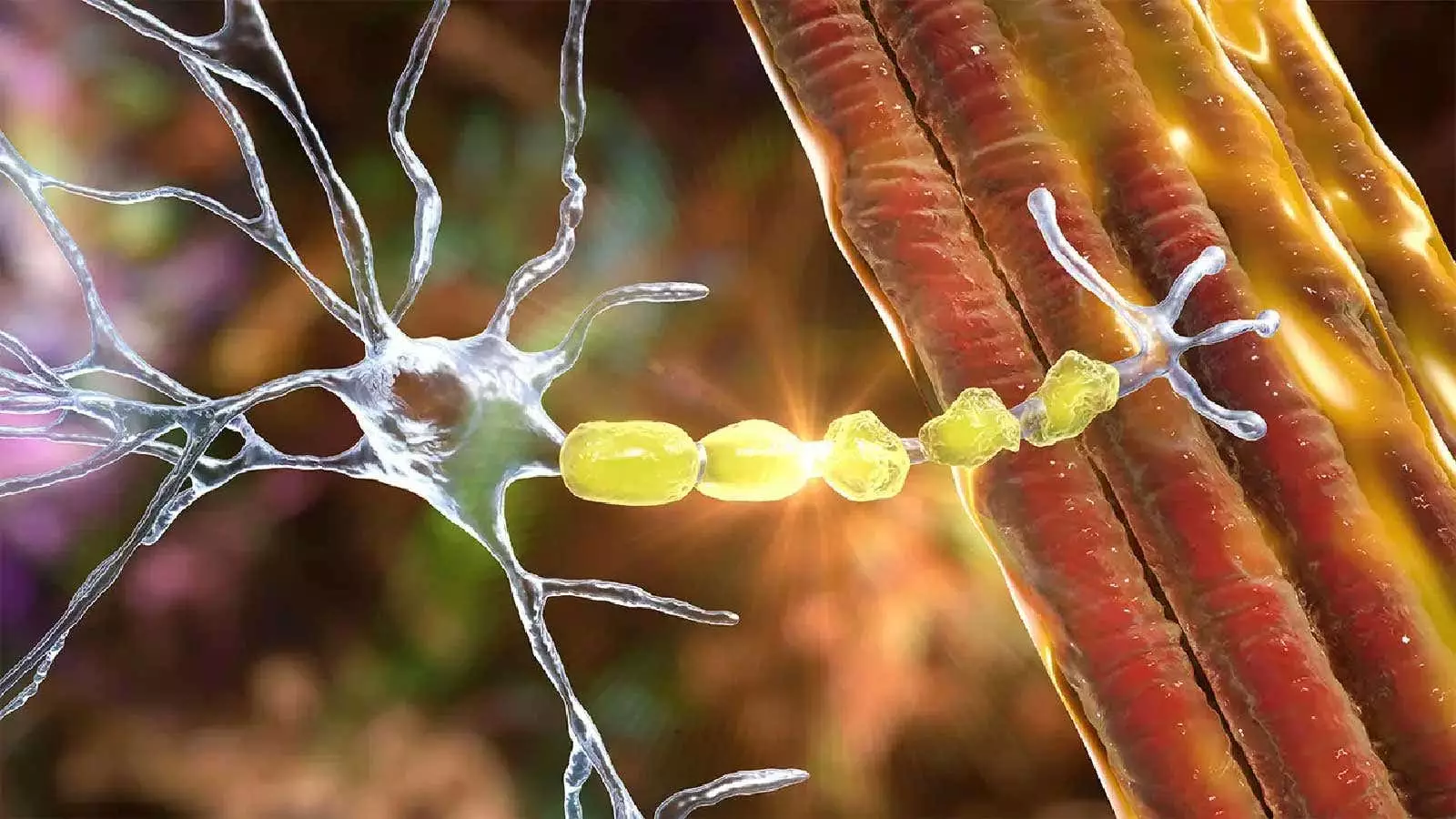
Over the years, researchers have been exploring various potential biomarkers for CIDP, such as autoantibodies, cytokines, complement proteins, Fc receptor modulators, and immunoglobulin G (IgG) levels. One of the promising biomarkers that have been identified is serum neurofilament light chain (NfL), which reflects axonal damage and is a predictor of poor outcomes in CIDP. Additionally, studies have shown that elevated levels of serum NfL are associated with disease progression in CIDP patients. Other biomarkers, such as anti-neurofascin-155 and anti-contactin-1 antibodies, have been found to be linked to relative resistance to IVIG therapy in patients with autoimmune nodopathies. These biomarkers could potentially help in making therapeutic decisions and monitoring disease progression.
In addition to fluid biomarkers, imaging biomarkers have also been explored in CIDP. Magnetic resonance neurography (MRN) has shown promising results in assessing nerve damage in CIDP patients. MRN offers high-resolution imaging that can provide clear images of nerve continuity, integrity, and pathological changes along the course of the nerve. Studies have demonstrated that MRN can detect thickening and increased T2 signal in affected nerves in CIDP patients as compared to healthy controls. This non-invasive imaging technique could play a crucial role in diagnosing and monitoring CIDP, especially in cases where traditional nerve conduction studies and electromyography are limited.
Ultrasound imaging has also emerged as a valuable tool in diagnosing CIDP. Researchers have shown that ultra-high frequency ultrasound of nerve structures can differentiate immune neuropathies like CIDP from controls. The European Academy of Neurology/Peripheral Nerve Society (EAN/PNS) guidelines recommend the use of ultrasound to diagnose CIDP in patients who meet the diagnostic criteria. Additionally, MRI has been suggested as a diagnostic tool for CIDP in adults with possible CIDP. These imaging techniques offer a non-invasive and detailed way to visualize nerve structures and assess their physical state, which can provide valuable diagnostic information in CIDP cases.
The search for biomarkers in CIDP is crucial for improving diagnosis, understanding disease activity, and guiding treatment decisions. The advancements in both fluid and imaging biomarkers offer new possibilities for accurately assessing CIDP and monitoring disease progression. Further research and clinical studies are needed to validate these biomarkers and integrate them into clinical practice for better management of CIDP patients.
Leave a Reply