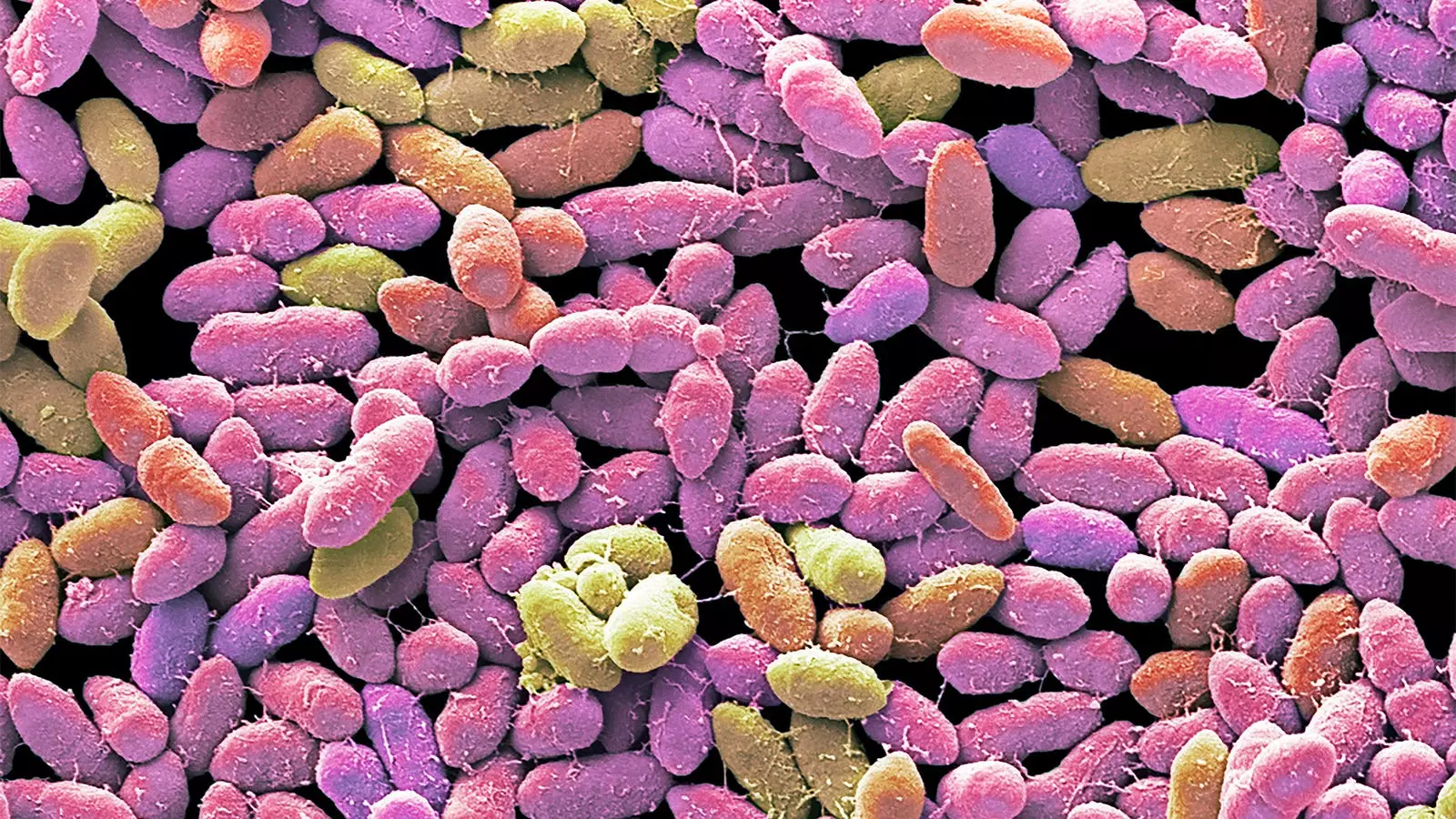
The American Gastroenterological Association (AGA) has taken a significant step by endorsing the use of fecal microbiota-based therapies for recurrent Clostridioides difficile infections (CDIs) in new guideline recommendations. However, the guideline advises against using such therapies for inflammatory bowel disease (IBD) and irritable bowel syndrome (IBS). The AGA guideline panel emphasizes that immunocompetent adults with recurrent CDIs should receive fecal microbiota-based therapies after completing treatment with standard-of-care antibiotics to prevent recurrence. On the other hand, mildly or moderately immunocompromised adults with recurrent CDIs are suggested to undergo conventional fecal microbiota transplant.
For adults hospitalized with severe CDI (defined by specific criteria) or those with fulminant CDI not responding to standard-of-care antibiotics, the panel recommends conventional fecal microbiota transplant. Such cases demand a multidisciplinary approach involving various medical teams to ensure comprehensive treatment. The guidelines highlight the importance of involving critical care, surgery, gastroenterology, and infectious disease specialties in managing severe or fulminant CDIs effectively.
In contrast to the endorsement for CDIs, the guideline panel explicitly advises against using fecal microbiota-based therapies for IBD and IBS due to a lack of current evidence supporting their efficacy in these conditions. Co-author Dr. Colleen Kelly emphasizes the importance of clinicians communicating this recommendation to patients inquiring about the use of such therapies for IBD or IBS.
The guidelines not only discuss the use of conventional fecal microbiota transplant via colonoscopy but also delve into recently FDA-approved therapies, like rectally administered fecal microbiota live-jslm and orally delivered fecal microbiota spores live-brpk. The authors provide detailed discussions and visual algorithms to aid in practical clinical decision-making regarding these therapies.
One significant concern highlighted in the guidelines pertains to the donor process for fecal microbiota-based products. The authors express reservations regarding the use of paid donors, as there may be a financial incentive for donors to misrepresent their health status or risk behaviors. This mirrors concerns raised in paid blood donation practices, where paid donors have shown a higher likelihood of having infectious diseases compared to voluntary donors.
Despite the endorsement and recommendations, the guidelines outline certain limitations and contraindications for fecal microbiota transplant. Patients with bowel perforation or obstruction, severe immunocompromised status, or specific medical conditions such as active cytotoxic therapy, CAR T-cell therapy, or untreated HIV infection are advised against undergoing such therapies.
It is important to note that while the AGA guidelines provide valuable insights and recommendations, all suggestions are conditional, backed by low- to very-low-certainty evidence. This underlines the ongoing need for further research and evidence to support the efficacy and safety of fecal microbiota-based therapies in various clinical settings.
Leave a Reply