Long COVID, a condition that affects individuals who have recovered from acute COVID-19 but continue to experience persistent symptoms, remains a mystery to researchers. However, a recent analysis of longitudinal data has shed light on potential factors underlying long COVID. In this study, blood samples from long COVID patients were analyzed, revealing significant changes to blood serum proteins that indicated activation of the immune system’s complement cascade, altered coagulation, and tissue injury.
The findings of this study, conducted by Dr. Onur Boyman and his colleagues from the University of Zurich, provide valuable evidence of an inflammatory signature specific to patients with active long COVID. Importantly, this signature was still detectable 6 months after symptom onset and independent of any information on COVID-19 history. These results have significant clinical implications, enabling more accurate diagnosis and potentially guiding treatment strategies for long COVID.
The exact underlying mechanisms of long COVID are still not well understood. Current hypotheses include tissue damage, viral reservoirs, autoimmunity, or persistent inflammation. The results of this study indicate a potential role for the complement system, a part of the immune system responsible for eliminating unwanted invaders. While the complement system is crucial for fighting infectious agents, chronic activation can cause collateral damage to blood vessels and tissues. Therefore, the study suggests that inhibitors of the complement pathway may hold promise in the treatment of long COVID.
The evidence implicating complement activation and thromboinflammation in long COVID aligns with previous research highlighting an increased propensity for clotting in individuals with long COVID. Dr. Ziyad Al-Aly, a researcher from the VA St. Louis Health Care System, emphasizes the importance of these findings in driving further investigation into biomarkers, diagnostics, and potential treatments for long COVID. The mechanisms of this condition are being elucidated rapidly, improving our understanding of the biology and providing hope for better management strategies.
To investigate the inflammatory signatures of long COVID, Boyman and his team followed 113 COVID-19 patients from Europe and the U.S., of whom 40 experienced long COVID symptoms at the 6-month follow-up. This group was compared to 39 healthy controls. Blood samples were collected at acute infection and again 6 months later. The researchers analyzed serum levels of 6,596 human proteins across all study participants.
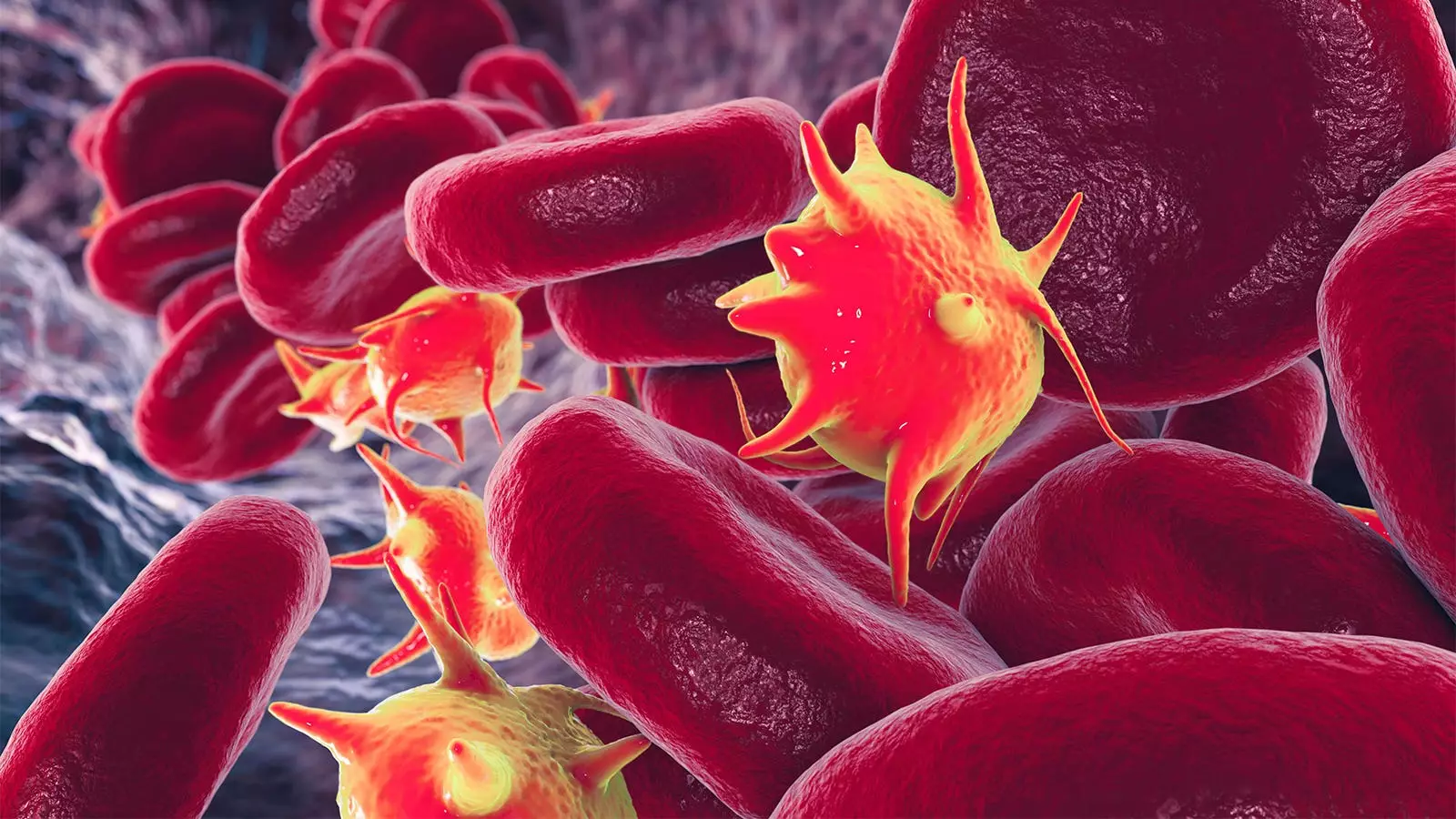
Comparing the long COVID patients, recovered patients, and healthy controls, the study identified serum biomarkers that were consistently elevated in long COVID at the 6-month mark. Most of these biomarkers overlapped with those altered in the subgroup of the cohort with severe acute COVID-19. Specifically, the long COVID patients exhibited elevated markers of tissue injury in their blood. Furthermore, they displayed a thromboinflammatory signature characterized by markers of endothelial activation, such as von Willebrand factor (vWF), and red blood cell lysis. At the cellular level, this signature was associated with increased monocyte-platelet aggregates.
Dr. Wolfram Ruf, an expert from the Johannes-Gutenberg University Medical Center and the Scripps Research Institute, suggests that the pathological features specific to long COVID offer potential opportunities for therapeutic interventions. While previous studies on acute COVID-19 treatment with coagulation and complement inhibitors have yielded mixed results, the distinctive features observed in long COVID patients warrant further investigation. Interestingly, microclots have also been observed in patients with myalgic encephalomyelitis-chronic fatigue syndrome (ME-CFS), indicating interplay between complement, vWF, and coagulation-mediated fibrin formation in postviral syndromes. Targeted coagulation inhibitors could potentially reprogram innate immune responses and disrupt the microangiopathic roles of vWF.
The study by Boyman et al. provides crucial insights into the inflammatory signature of long COVID and the potential role of blood proteins in its pathogenesis. By identifying specific changes in blood serum proteins associated with complement activation, altered coagulation, and tissue injury, this research opens new avenues for diagnosis and treatment. As our understanding of long COVID continues to evolve, it is becoming increasingly clear that a multi-faceted approach is needed to unravel its complexity and develop effective interventions.
Leave a Reply