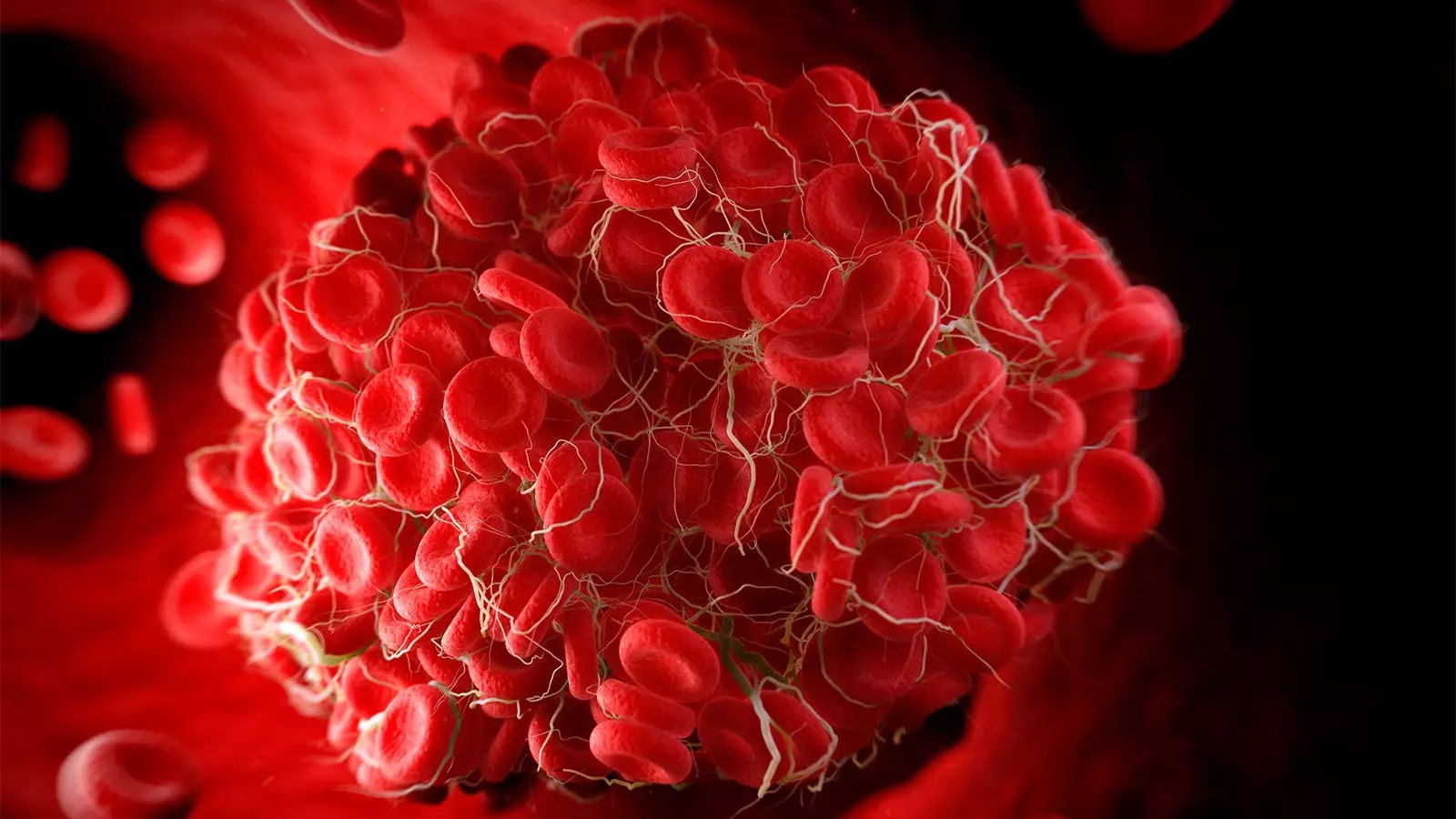
Pulmonary embolism (PE) remains a significant cause of mortality in hospitalized patients, particularly among those with high-risk PE. A recent analysis of the Pulmonary Embolism Response Team (PERT) Consortium Registry revealed alarming findings regarding the outcomes of high-risk PE patients. This article critically examines the study conducted by Jay Giri, MD, MPH, and co-authors, shedding light on the high mortality rates and other risk factors associated with high-risk PE.
The retrospective analysis included nearly 5,800 patients, demonstrating considerably higher in-hospital mortality rates among high-risk PE patients compared to those with intermediate-risk PE. The study revealed a mortality rate of 20.6% in high-risk PE patients, which although lower than previous observational studies, is still alarmingly high. It is worth noting that these statistics could be influenced by the more comprehensive data capture, improved technology, and enhanced care delivery methods in experienced PERT centers.
PE continues to be one of the leading causes of cardiovascular death in the United States. Behnam N. Tehrani, MD, and co-authors emphasize the imperative need for universally accepted definitions of high-risk PE and advancements in risk assessment models. Studying the signals of efficacy, such as durable changes in hemodynamics, metabolic measures of tissue perfusion, and predictive factors for myocardial recovery, could aid in improving patient outcomes and reducing mortality rates.
The multivariable regression analysis conducted in this study identified several factors associated with increased in-hospital mortality among high-risk PE patients. These factors included vasopressor usage, extracorporeal membrane oxygenation (ECMO) use, the presence of clot-in-transit, and malignancy. Understanding these risk factors can assist healthcare providers in implementing appropriate interventions and personalized treatment strategies for high-risk PE patients.
The study also highlighted the increased mortality rates and utilization of specific interventions in patients with catastrophic PE. Patients with catastrophic PE had significantly greater in-hospital mortality compared to non-catastrophic cases. Furthermore, ECMO and systemic thrombolysis were more commonly employed in catastrophic PE cases. These findings emphasize the urgent need for early identification and prompt management of catastrophic PE to improve patient outcomes.
While the analysis provides important insights, it is crucial to acknowledge the limitations of the study. The data were obtained from the PERT Consortium Registry, which might have excluded patients who did not receive prior consultations associated with the registry. Additionally, the length of stay and intensive care unit utilization might have been influenced by the utilization of advanced therapies, potentially affecting the study’s outcomes.
The study conducted by Jay Giri, MD, MPH, and co-authors sheds light on the high mortality rates among patients with high-risk PE, highlighting the urgent need for improved risk assessment models, universally accepted definitions, and novel metrics to enhance patient outcomes. Recognizing the factors associated with increased mortality and utilizing appropriate interventions can make a significant difference in the management of high-risk PE cases. With further research and advancements, healthcare providers can strive to reduce PE-related mortality rates and ensure better patient care.
Leave a Reply