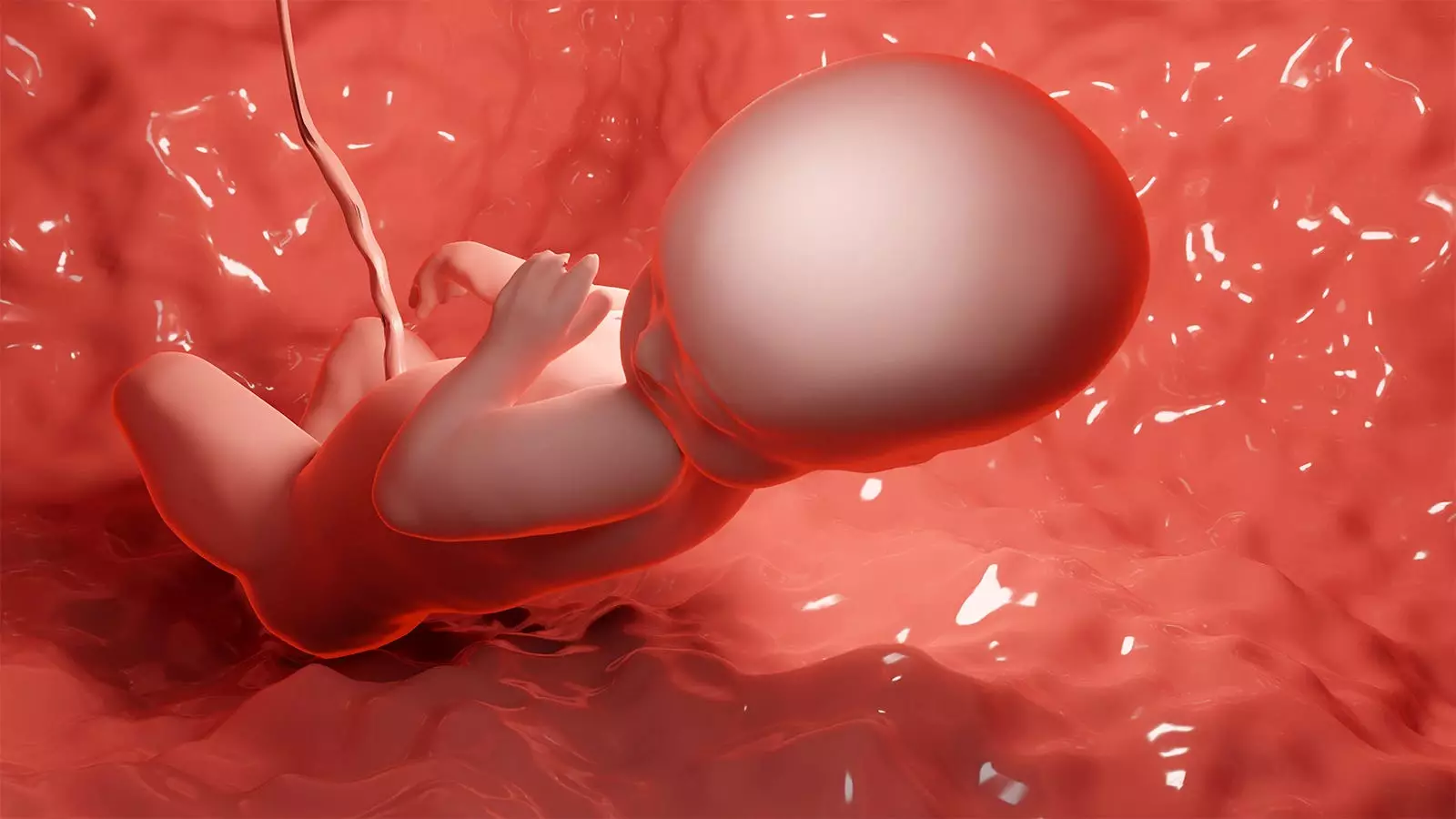
In a groundbreaking study known as the RAFT trial, researchers have made significant progress in the treatment of fetal renal agenesis, a condition that has previously been uniformly lethal. Serial infusions of amniotic fluid were used to restore lost amniotic fluid due to the lack of fetal renal development before 26 weeks’ gestation. The results of the study showed an improved rate of live births without maternal safety risks. However, while this trial provides hope for the future, it also highlights the challenges in managing kidney disease complexities for these patients in the long term.
The RAFT trial focused on 18 cases of fetal bilateral renal agenesis, a severe congenital anomaly of the fetal urinary tract. Out of these cases, there were 17 live births, resulting in a 94% live birth rate at a median gestational age of 32 weeks. Additionally, 14 of these infants survived to at least day 14, meeting the primary outcome of the trial. Factors associated with survival to 14 days included a higher number of amnioinfusions, gestational age greater than 32 weeks, and higher birth weight. It is important to note that no serious maternal complications occurred during the trial. However, the trial was stopped early due to concerns about potential harm and the burden of morbidity in longer-term survivors, especially stroke.
The findings of the RAFT trial have significant implications for prenatal counseling. Previously, bilateral renal agenesis was considered a condition with zero chances of survival. However, this trial has shown that survival is possible with serial amnioinfusions. Prenatal counseling will now have to include this new information, providing hope to families facing this diagnosis. However, it is noted that parental interviews were not conducted as part of the trial, which could have provided valuable insight into the families’ perspectives. To address this, a qualitative study is planned to better understand the families’ experiences and guide future prenatal counseling.
While the RAFT trial has opened doors to potential survival for infants with bilateral renal agenesis, it also highlights the challenges in managing kidney disease complexities for these patients in the long term. Only 35% of the neonates survived to hospital discharge with placement of long-term dialysis access. Out of these survivors, there were cases of infectious complications, cardiac arrest, and strokes. The researchers acknowledged that the trial could not solve the challenge of managing kidney disease complexities in the long term.
Moving forward, further research is needed to address the complexities of neonatal management for babies born without kidneys or with other forms of fetal renal failure. The successful results of the RAFT trial have created a new cohort of babies that did not exist before, requiring specialized and tailored approaches to neonatal care. This presents an opportunity for future research and advancements in the field.
It is important to acknowledge the limitations of the RAFT trial. The study was nonrandomized and had a small sample size. This calls for caution in generalizing the findings to a larger population. Additionally, there was a lack of diversity in the study population, which may limit the applicability of the results to different demographics.
The RAFT trial has paved the way for progress in the treatment of fetal renal agenesis, demonstrating that serial amnioinfusions can improve the chances of live births in cases that were previously uniformly lethal. However, the challenges of managing kidney disease complexities in the long term remain. The findings of the trial have important implications for prenatal counseling, providing hope to families facing this diagnosis. Future research should focus on the neonatal management of babies born without kidneys or with other forms of fetal renal failure prenatally, to address the unique challenges they face. While the RAFT trial is a significant step forward, continued research and advancements are needed to improve outcomes for these patients and their families.
Leave a Reply