In the relentless search for solutions to Alzheimer’s disease, recent studies indicate that we may be on the brink of a significant breakthrough. The reality of our aging population—and the accompanying rise in neurodegenerative diseases—compels us to innovate and think critically about preventive measures. Researchers are now cautiously optimistic that methods to slow down the progression of Alzheimer’s in diagnosed patients could also stall the disease’s onset in those genetically predisposed to it. Randall J. Bateman, a prominent neurologist from Washington University, embodies this hope with his declaration that we might soon be able to delay Alzheimer’s for millions.
This excitement, however, is tempered by the serious complexities inherent in Alzheimer’s research. The focus of recent trials has been specifically on individuals with Dominantly Inherited Alzheimer’s, which, despite accounting for only 1% of all cases, guarantees that those affected will likely develop the condition by their 50s due to a genetic mutation that accelerates amyloid protein production. This highlights not just medical urgency but also the moral imperative to develop actionable strategies for prevention.
The Journey of Gantenerumab
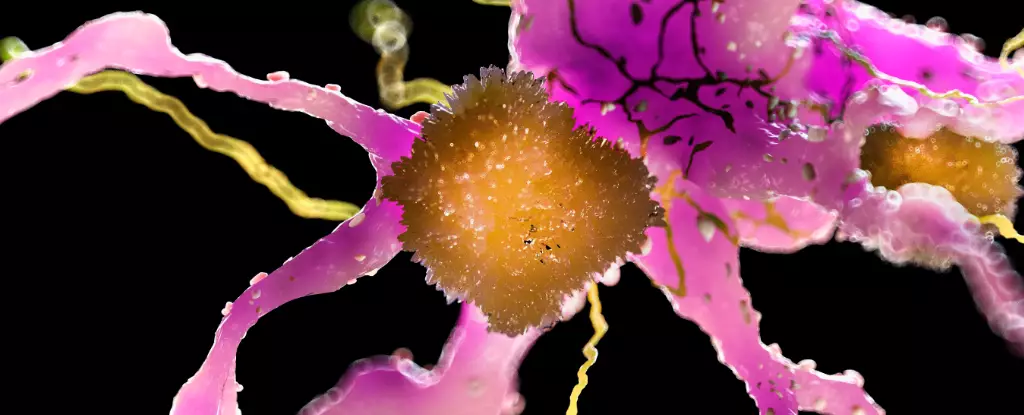
The drug in question, gantenerumab, was previously involved in a phase 3 clinical trial targeting individuals with minimal cognitive decline. While it ultimately fell short in alleviating symptoms for those already symptomatic, a silver lining emerged: the drug demonstrated meaningful improvement in reducing pathological markers associated with Alzheimer’s. This led to further exploration of higher dosages and the possibility of expanded use among participants with high-risk genetics, who, despite being initial placebo recipients, were given the opportunity to try the drug.
What is compelling here is not only the gradual forging of progress from apparent setbacks but also the relentless pursuit of understanding the nuances of Alzheimer’s pathology. The most striking result from continued administration of gantenerumab is that it appears to have halved the risk of developing symptoms in those who had previously been deemed destined for cognitive decline. It raises a tantalizing possibility: could this drug be the first glimpse into a preventive future where Alzheimer’s is delayed, if not entirely avoided?
The Dark Side of Innovation
Nevertheless, the discussions surrounding gantenerumab deserve a deeper exploration of the ethical considerations that govern its use. The responsibility to weigh the potential benefits against the risks, which include cerebral microbleeds and an uptick in brain swelling, cannot be overstressed. It is alarming how such treatments, meant to prolong life and enhance cognitive function, might also pose severe risks. As we progress toward rethinking Alzheimer’s treatment and prevention, we must rigorously scrutinize both the immediate effects and long-term implications.
This dichotomy of hope and fear is at the forefront of medical research, particularly in the context of anti-amyloid therapies. While the approval of other next-generation treatments in the U.S. signifies progress in caring for symptomatic patients, the same innovative spirit must be applied to developing safe, preventive measures for those at risk.
Imagination Meets Reality
What does all this mean for the future and for those genetically at risk of Alzheimer’s? As we stand at the intersection of hope and potential despair, the prospect of living longer with healthy cognitive faculties is becoming less of a dream and more of a tangible reality. Yet, maintaining a balanced perspective is vital. We need a dialogue that not only champions innovation in medicine but acknowledges the roadblocks trailing behind such advancements.
As researchers labor tirelessly to refine their approaches, the conversations surrounding Alzheimer’s must evolve to include a broader societal context. It is no longer about merely treating those already affected but about embarking on a preventive revolution that could redefine our understanding of aging and cognitive decline. The emergence of trials suggesting that treatment can delay symptoms might pave the way for policies and programs aimed to protect future generations from the ravages of Alzheimer’s.
In building this future, a collective acknowledgment of ethical boundaries and potential risks must guide our steps. The public deserves a clear view of the landscape—a landscape filled with both peril and promise. By facilitating transparent discussions, investing in continuous research, and fostering community awareness, we might find ourselves leading not just innovations in treatment but also in redefining what it truly means to live with Alzheimer’s or, better yet, to avoid it altogether.
Leave a Reply